Curs 6 Sd Mal Absorb Tie
-
Upload
delia-wuchti -
Category
Documents
-
view
245 -
download
7
description
Transcript of Curs 6 Sd Mal Absorb Tie
-
SINDROMUL DE MALABSORBIE
-
SINDROMUL DE MALABSORBIE Sindromul de malabsorbie reprezint totalitatea simptomelor care apar ca urmare a tulburrilor enzimo-digestive intraluminale i/sau a tulburrilor de captare, transport i livrarea spre circulaia sanguin sau limfatic a unuia sau mai multor produi terminali ai digestiei intraluminale precum i a substanelor minerale i vitaminelor.
-
Noiuni de anatomie i fiziologie a intestinuluiIntestinul subire se ntinde pe o lungime de peste 4 m la adult, de la nivelul duodenului, pan la nivelul valvulei ileo-cecale.Jejun-ileonul este situat n spaiul visceral al cavitii peritoneale, fiind nvelit de seroasa peritoneal.Arterele provin din trunchiul celiac i din artera mezenteric superioar.Venele nsoesc arterele i dreneaz n vena port.Limfaticele formeaz o reea mucoas, care prin reele succesive dreneaz n trunchiul intestinal i apoi n cisterna Pequet.Mucoasa intestinal prezint numeroase pliuri cu viloziti intestinale i cripte, care i confer o mare suprafa aditional.Procesul de absorbie intestinal are loc la nivelul epiteliului intestinal.
-
Procesul de digestie i absorbie se poate diviza n 3 etape succesive:1.
Digestia sau transformarea glucidelor, lipidelor i proteinelor n constituieni absorbabili. Acetia sunt pentru :glucide - diferite monozaharide (hexoze,pentoze),lipide - acizii grai i monogliceridele,proteine - aminoacizii.2. Procesul de traversare a mucoasei intestinale.3.Transferul acestor compui n vase sanguine (vena port sau limfatice) spre ficat.
-
Absorbtie
Pasajul prin epitelul intestinal cu viloziti care mresc suprafaa de absorbie se face printr-un :- mecanism pasiv = difuziune ex. fructoza, apa, Cl, K+, HCO3,-mecanism de transport activ cu transportori sau enzime specifice.Procesul consum energie, de exemplu pentru aminoacizi, monozaharide - glucoza, galactoza.- absorbie facilitat un mecanism similar difuziunii pasive, dar mediat de transportori.
-
Glucidele
Cele mai multe sunt ingerate sub form de amidon, care sub influena amilazei salivare i pancreatice este hidrolizat n oligo- apoi n dizaharide. La nivelul marginii n perie a enterocitelor dizaharidazele sunt descompuse n monozaharide, absorbite i apoi transportate spre circulaia portal.
-
Specific enzymes secreted by cells in the wall of the small intestine break down the complex sugars into glucose and a small amount of other simple sugars. Sucrose, ordinary table sugar, is an example of a complex sugar. The sucrose molecule is composed of two six-carbon sugars bonded together. The final result of most carbohydrate digestion is glucose(6C), the carbohydrate that cells can use in respiration., Others sugars are produced that have five carbon atoms. Ribose is an example of a five-carbon sug
-
Proteinele i aminoacizii
Proteinele sunt degradate iniial n stomac sub aciunea pepsinei, care este completat apoi de tripsina i chimotripsina pancreatic ca i de alte endo- sau exopeptidaze, - oligopeptide, dipeptide i aminoacizi. Similar dizaharidazelor, exist dipeptidaze localizate att n citoplasm ct i n marginea n perie a epiteliului intestinal, ce acioneaz asupra dipeptidelor, care sunt ulterior transportate activ prin mecanisme distincte spre circulaia portal
-
Majoritatea grsimilor ingerate sunt trigliceride(acizi grai i glicerol). Sub aciunea lipazei i a co-lipazei pancreatice monogliceride i acizi grai, micelii mixte, prin care sunt solubilizate grsimile i este favorizat absorbia lor.
Lipidele
-
Lipidele
Monogliceridele i acizii grai cu lan lung sunt reesterificai n trigliceride la nivelul enterocitului, apoi interactioneaz cu apo-lipoproteine specifice pentru a forma chilomicroni si VLDL, alturi de colesterol i fosfolipide, form sub care sunt secretate n vasele limfatice i ajung apoi n ficat.Acizii grai cu lan mediu (C8-C12) nu sunt reesterificati i nglobai n chilomicroni, ei ptrunznd direct n sistemul venos portal i fiind transportai n plasm legai de albumin.
-
Fat DigestionDuodenumJejunumIleumColonBiliary Transport and StorageLiver
-
Fat DigestionTriglyceridesDietary CholesterolFatty Acids + MonoglyceridesLipaza pancreatica
-
Triglyceride AbsorptionLymphEnterocyteIntestinal Lumen2 Fatty Acid+MonoglycerideDGATTriglyceride
-
Chylomicron FormationLymphEnterocyteIntestinal LumenCholesteryl EsterCMapoB48Triglyceride
-
Cholesterol AbsorptionMicellar particle comes in the proximity of an enterocyte, cholesterol is transported into the enterocyte through a channel recently identified as NPC1L1.A fraction of this cholesterol is pumped back out of the enterocyte into the intestinal lumen by the complex ABCG5/G8A fraction of cholesterol is esterified by the enzyme acyl-coenzyme A: cholesterol acyltransferase (ACAT)
-
Biliary and Dietary CholesterolDuodenumJejunumIleumColonBiliary Transport and StorageFecal excretion (1.2 g/d)Dietary Cholesterol (0.4 g/d)Absorption ~50%CMapoB48LiverBiliary Cholesterol (2 g/d)
-
Cholesterol AbsorptionLymphEnterocyteIntestinal LumenCholesterolNPC1L1Cholesteryl EsterABCG5/G8ACAT
-
Reverse Cholesterol TransportBloodPeripheral TissuesLiverBileExcess Cholesterol
-
Cholesterol BalanceDuodenumJejunumIleumColonBiliary Transport and StorageCholesterolCholesterol (1.2 g/d) + Bile Salts (0.4 g/d)Dietary Cholesterol (0.4 g/d)Loss (1.6 g/d)Bile saltsLoss (1.6 g/d) Dietary Cholesterol (0.4 g/d)Synthesis (1.2 g/d)Liver
-
Cholesterol Absorption InhibitorsDuodenumJejunumIleumCMapoB48Liver/ statineCM Remnant apoB48VLDL apoB100LDL apoB100Colon
-
Aceste procese pot avea loc pentru unele substane pe toat lungimea intestinului subire,Pentru unele substane exist suprafee/regiuni limitate ex. pentru vitamina B12 i acizii biliari ileonul terminal.Intestinul proximal constituie sediul principal pentru fier, calciu, vitamine hidrosolubile i grsimi (monogliceride i acizi grai)Sediul absorbiei
-
Sediul absorbiei
Aminoacizii sunt absorbii mai mult la nivelul intestinului mijlociu (in jejun)
Glucidele sunt absorbite att n intestinul proximal ct i n cel mijlociu.
-
Maldigestiase refer la tulburarea proceselor enzimo-digestive intraluminale.Tipuriinsuficien de secreie a enzimelor digestive- aclorhidrie- boli pancreatice (lipaz, amilaza, tripsin)- carene dizaharidice .-deficit de stimulare a secreiei enzimatice:- aclorhidrie,- scurt circuitarea duodenului (ex.stomac rezecat
-
Maldigestiamodificarea parametrilor optimi de activitate a enzimelor- ex n s. Zollinger-Ellison prin pHul acid se inactiveaz enzimele pancreatice, se produce precipitarea acizilor biliari i formare deficitara de micelii;- lipsa unor factori de activare enzimatic ex.-deficitul de sruri biliare din hepatopatiile cu sindrom colestatic, intreruperea circuitului entero-hepatic al srurilor biliare- ex rezectii ileale, boli inflamatorii intestinale ca boala Crohn utilizarea unor medicamente care fixeaz srurile biliare (ex. colestiramina)-
-
Maldigestiaaccentuarea tranzitului intestinal maldigestie prin lipsa de timpex-intestin scurt, rezecie gastric.-asincronismul dintre prezenta chimului alimentar i secreiile enzimatice ex stomacul operat tip Bilroth II
-
.2. Malabsorbia
Este legat de alterarea funciilor mucoasei intestinale i a celulelor epiteliale intestinale(enterocite).Malabsorbia se refer la tulburarea mecanismului de transport spre cile sanguine/limfatice.Malabsorbia se poate produce prin:- a. Reducerea suprafeei de absorbie -ex rezecii intestinale, bypass intestinal- b. Tulburarea metabolismului intracelular a enterocitului ex. abeta-lipoproteinemia- c. Blocarea transportului intracelular i a procesului de eliberare a substanelor absorbite
-
2.Malabsorbia
Exist malabsorbii : a.- globale pentru toate principiile alimentare,b.- selective prin deficite de absorbie specifice- n bolile genetice care afecteaz aminoacizi, monozaharide (ex.carene de dizaharidaze)
-
3.Exudaia endo-intestinal
Procesul exudativ, care este maxim pentru proteine, dar este prezent i pentru lipide sau electroliti. Se ntlneste n numeroase enteropatii, dar exudatia endo-intestinal se ntlnete cel mai frecvent cnd:
- exist un obstacol pe cile limfatice ex.n insuficiena cardiac dreapt, pericardita constrictiv, B.Wipple, TBC intestinal, limfoame intestinale;- n distrofia reelei limfatice mezenterice- ex. limfangiectazia intestinal- afeciuni intestinale cu leziuni distructive ale epiteliului intestinal- ex. colita ulceroas, boala Crohn.
-
4.Populare bacteriana intestinal n mod normal intestinul subire proximal este steril prezentnd sub 104 germeni/ml (B.Colli n aerobioz)Statusul bacteriologic normal este denumit eubioz.n condiii patologice apare disbioza populare cu germeni anaerobi (de tip fecal) care:- 1. modific mucoasa > atrofie vilozitar- 2. deconjug sruri biliare > tulburarea absorbtiei lipidelor- 3. consum competitiv hidraii de carbon
n final, prin aceste mecanisme rezult un deficit nutriional, de vitamine, de proteine i grsimi care caracterizeaz sindromul de malabsorbie
-
Clasificarea sindromului de malabsorbie1.Sindromul de malabsorbie prin tulburare de digestie intraluminalGastric -Rezecii gastrice tranzit rapid, tulburri de mixic i asincronism de evacuare ex. gastrectomia tip Billroth II - Sindromul Zollinger-Ellison modificrile pHului duodenal - aclorhidriePancreas Insuficiena pancreatic exocrin- deficite de enzime pancreatice izolate: lipaza, co-lipaze,- fibroz chistic- pancreatit cronic,- cancer pancreatic
-
Sruri biliare Scderea concentraiei intraluminale de acizi biliari- boli hepatice severe- colestaza intra- i extrahepatic- fistule biliare (colecistocolonic)- deconjugarea srurilor biliare- n sindromul de intestin subire contaminat- precipitarea i sechestrarea srurilor biliare neomicin - colestiramin - sruri de Al i Mg2. Micorarea suprafeei de absorbie intestinal- afeciuni inflamatorii ex. B-Crohn, ileita de iradiere- by- pass ileal- rezecie ileal
-
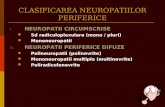
II. Sindromul de malabsorbie prin tulburri de absorbie1. Malabsorbii ereditare selective la copiiB.Hartnup pentru aminoacizi neutriCistinuria pentru aminoacizi dibazici (lizin, ornitin, arginin) Iminoglicinuria Malabsorbia metioninei Malabsorbia triptofanului boala scutecelor albastre Deficit congenital de Factor IntrinsecMalabsorbia primar a vitaminei B12- sindrom Imerslund
-
2. Malabsorbii ereditare globale: boala incluziilor microvilozitare3.Boli prin mecanismul de hipersensibilizare sau imunologic- enteropatie glutenic- enteropatie alergic4. Boli prin suprapopulaie bacterian- sindromul intestinului subire contaminat- B.Whipple- TBC intestinal- Sprue tropical5. Parazitoze- Giardia lamblia- Strongyloides stercoralis
-
6. Carene dizaharidice primare sau secundare-deficit de lactaz-deficit de dizaharidaze7. Boli inflamatorii sau infiltrative-amiloidoza-limfoame8. Obstacol n drenaj limfatic-limfangiectazia intestinal-Boala Wipple-TBC intestinal-limfoame9. Fibroze:-scleroz sistemic (sclerodermie)-enterite de iradiere
-
Manifestri clinice:
1.De tip sindrom carenial Deficit ponderal pna la caexie, IMC < 18 20Kg/m Astenie, reducerea capacitii de efort Depresie psihic Hipotensiune arterial ortostaticCel mai adesea- sindrom diareic cu aspect de steatoree
-
2. Semne de carene vitaminice
B1 nevrite periferice, boala beri-beriB2- (asociat cu deficit de folai, Fe) glosit, stomatit, cheilitB12 (asociat cu deficit de folai) anemie macrocitar, megaloblasticDeficit de B+PP pelagra gastrogen sau enterogen.n afeciunile cu steatoree rezult un deficit de vitamine liposolubile.Vitamina A- hemeralopie, hiperkeratoz folicularVitamina D- osteopatie, osteomalacieVitamina K sindrom hemoragipar
-
Modificri tegumentarePacienii sunt palizi:- Prin lipsa de fier anemie microcitar- lipsa B12, folai anemie macrocitarEczemeManifetri purpuriceHiperkeratoz i dermatit folicular
Manifestri musculo-scheletice-dureri osoase prin depletie proteic, osteoporoz i osteomalacie-osteoartropatie- tetanie, parestezii- prin malabsorbie de calciu, magneziu
-
Tulburri hidrominerale- sindrom de hipocalcemie spasmofilie, tetanie- sindrom de hipomagnezemie, astenie, palpitaii;- scderea Zn- acrodermatita- sindrom de deshidratare- acidoza metabolic- respiraie Kussmaul
Hipoproteinemie edeme atrofii musculare
-
Deficite hormonale hipopituitarism tulburare de cretere (nanism, infantilism) hipogonadism: amenoree, scderea libidoului insuficien corticosuprarenalSistem nervos-scderea vederii nocturne-neuropatie periferic
-
Laborator
Majoritatea testelor utile in diagnosticul malabsorbiei indic prezena unei funcii deficitare de absorbie sau de digestie, dar numai puine dintre acestea sugereaz un diagnostic specific.De aceea pentru stabilire diagnosticului este necesar efectuarea unor combinaii de teste.Teste pentru malabsorbie:-analiza grsimilor n fecale calitativ coloratie cu Sudan III cantitativ >6g/24h testul de absorbie excreie al XilozeiD-xiloza glucid care se absoarbe total n intestin i se excret n ntregime n urin. Se administreaz 25g xiloza N se excret peste 4,5g la 5h.n malabsorbie-
-
Examen baritat gastro-intestinal-aspectul stomacului, intestinului, (pliuri, tranzit)- Endoscopia pentru tractul digestiv superior-Biopsia de intestin subire cu dozare histochinic de enzime- Test Schilling pentru absorbtia Vit. B12-Timpul de protrombin deceleaz malabsorbiei vit.K; se corecteaza dup administrare de vit K parenteral.- Teste biochimice - Proteine totale, albumine, lipide, colestesterol electrolii - Ca, Mg, Fe.- Pentru flora intestinal exacerbat test respirator cu C*- Testul la secretin i alte teste pancreatice.
-
Diagnostic pozitiv cuprinde mai multe etape:
- Recunoaterea sindromului de malabsorbie clinic, laborator -Precizarea mecanismului patogenetic - Precizarea bolii de baz.
-
Tratament-Msuri cu caracter etiologic-Pentru infestaii parazitare tratament specific ex pentru lambliaz tinidazol -Restricii alimentare pentru alergii alimentare ex. Glutenul din gru n enteropatia glutenic.-Corectarea deficitelor vitaminice-Vitamina A 100 000UI/sptmn, apoi 100 000UI la 3 luni-Vitamina D 100 000UI/ sptmn, apoi lunar;-Vitamina K 10mg/zi-Vitamina E 300mg/zi-Suplimentarea lipidelor cu trigliceride cu lan mediu-
-
Tratamentul osteoporozei cu alendronat sodic (Fosamax) sau calcitonin cu suplimentarea calciului calciu lactic 1000mg/zi per os. - Corectarea insuficienei pancreatice- cu enzime pancreatice n preparatale Kreon, Zymogen,Triferment - Corectarea deficitului de HCl soluie de HCl, acidopeps - Corecia anemiei
-
Tratament antibacterian- Obiectiv-restabilirea eubiozei intestinale- Identificarea germenilor prin coprocultur- Antibiotice cu spectru larg Furazolidon, Derivai chinolonici Ciprofloxacina 2x500mg-Administrarea de tulpini orale de Bacilus Bifidus, Bacilus lactis, Bacilus subtilis 4-6cps/zi.Tratament antiinflamator i imunomodulator n boala Crohn, rectocolit ulcerohemoragic tratament cu Salozopirina, corticoterapieCorectarea hiperperistaltismului : cu loperamid (Imodium), anticolinergice
-
ANOMALII GENETICE SAU BIOCHIMICEEnteropatia glutenic (Sprue celiac)Enteropatia produs de gluten mai este denumit la copil sprue celiac, boal celiac , sprue netropicalGlutenul este o substan proteic care se gsete n finoase (paste, pine, gru,fidea)- boala apare n climat temperat, mai frecvent la femei- are caracter familial- incident crescut a antigenelor HLA tip DR3 (la 70-90% din cazuri) si HLA- DQw2
-
Patogenez
Glutenul i gliadina sunt proteine cu mas molecular mare, prezente n special n gru. Mecanismul exact de producere al bolii este necunoscut.Exist o teorie toxic ce presupune lipsa unei peptidaze care scindeaz glutenul, care se acumuleaz n mucoasa intestinului cu efect toxic.A doua teorie presupune un mecanism .imunologic glutenul ar avea un efect inflamator local.
-
Morfopatologie
Aspectul caracteristic este de atrofie sau subatrofie vilozitar- mucoas intestinal cu aspect plat.- localizarea leziunii : expresie maxim n duoden i jejun- infiltrat cu limfocite, plasmocite n lamina propria-reversibilitate leziunnilor la excluderea glutenului reprezint un element fundamental pentru diagnostic.
-
Semne clinice
Boala are expresie clinic variat.
Boala poate debuta n copilrie sau cnd se introduc la sugar finoasele.- Diaree cu aspect steatoreic,dar si scaune apoase la 1-2h dup ingestia de finoase, apar apoi i alte intolerane alimentare la lapte, cruditi, dulciuri.- Scdere n greutate- Tegumente uscate, pelagroide, fenomene polinevritice, anemii, retardare staturo-ponderal- Triada celiac- Diaree - Slbire - Abdomen voluminos
-
Enteropatia glutenic a adultului
Simptomul major este tot diareea, de obicei cu aspect steatoreic, intlnit n 66-90% din cazuri. Tulburrile de tranzit sunt accentuate de eforturi fizice excesive, stres psihic, alimentatie bogat n grsimi.Alte semne: pierdere ponderal, dispepsie gazoas, greturi, vrsturi, dureri abdominale moderate
-
Diagnostic pozitiv
- Existena unei malabsorbii (clinic, teste de laborator)-Detectarea unor anticorpi specifici: atc antigliadin, antiendomissium si antireticulin- Biopsie jejunala atrofia vilozitilor- Ameliorarea bolii dup suspendarea glutenului din alimentatie- Endoscopic- la nivelul Duodenului II reducerea/dispariia pliurilor mucoasei.Test de provocare cu 30-50g gluten pe zi, pe cale oral, iar dac apare brusc diaree cu steatoree se poate confirma diagnosticul de enteropatie indus de gluten.
-
Tratament
- Regim fr gluten amelioreaz 80% din pacieni este permis orezul i derivatele, cartof, porumb, soia, ovz)- Corticoizi-Tratament substitutiv pentru vitamine, minerale, anemie
-
Enteropatii prin deficite dizaharidice
Hidroliza dizaharidelor se petrece la nivelul marginii n perie a celulelor epiteliului intestinal prin aciunea unor enzime numite dizaharidaze sau monozaharidaze specifice.Deficitul de lactaz la adultReprezint intolerana fa de lactoz, principalul dizaharid al laptelui.Lactoza neabsorbit din intestin are efect osmotic, atragnd lichid n lumenul intestinal, determina iritaie > diaree.Scaunul datorit fermentaiei lactozei contine acid lactic i are pH acid.
-
Simptome
Simptomele apar la 30-40 min. dup ingestia de lapte, care determin meteorism, crampe, flatulent, diaree.Majoritatea pacienilor tiu c nu tolereaz laptele i il evit.
-
Test de toleran la lactoz
Se administreaz 50g lactoz in 400ml ap la adultLa copil 1-2g/kg corpClinic la 10-15 dup ingestie apare sindromul de intoleran precoce.Coprologic emisie de scaune apoase cu pH acid.La cromatigrafie in supernatant exist lactoz nescindatBiologic- se recolteaz glicemia la 0- 60- 120Normal exist o cretere cu peste 20% fa de valoarea iniial, care nu apare la aceti pacieni.
-
Deficitul dobndit de lactazasociat cu o varietate de boli gastrointestinale cum ar fi boala Crohn, infecii virale i bacteriene ale tractului intestinal, lambliaz, abetalipoproteinemia, fibroza chistic etc.
As shown by the white box, fat digestion occurs in the lumen of the small intestine and is facilitated by these micellar particles.Fat in the diet consists of cholesterol as well as triglycerides. Dietary cholesterol is incorporated into micelles together with the biliary cholesterol that was already present. Dietary triglycerides are partially broken down by pancreatic lipases into fatty acids and monoglycerides, which are also incorporated into micellar particles.Triglycerides are assimilated into the body by the separate absorption of fatty acids and monoglycerides, which are re-esterified by the enzyme acyl-coenzyme A:diglycerol acyltransferase (DGAT) to form triglycerides.Triglycerides and cholesteryl esters are incorporated, together with apolipoprotein (apo) B-48, to form chylomicron particles, which are exocytosed into the lymph and then enter the circulation.Cholesterol is secreted into bile at the rate of up to 2 g/day. The average American diet consists of about 0.4 g/day of cholesterol. Therefore, the amount of cholesterol that is derived from bile in the intestine is up to 5-fold in excess of the amount that is taken in through the diet. The biliary cholesterol and dietary cholesterol are admixed in the intestine to form a pool of cholesterol molecules that are indistinguishable. The average individual absorbs 50% of the cholesterol that passes through the intestine each day. This means that 50% is lost in the feces, amounting to 1.2 g/day.There are three main points of regulation for cholesterol absorption into the body. When the micellar particle comes in the proximity of an enterocyte, cholesterol is transported into the enterocyte through a channel recently identified as NPC1L1. A fraction of this cholesterol is pumped back out of the enterocyte into the intestinal lumen by the complex ABCG5/G8, and the remainder is esterified by the enzyme acyl-coenzyme A:cholesterol acyltransferase (ACAT) into cholesteryl esters.
Reference:Altmann SW, Davis HR Jr, Zhu LJ, Yao X, Hoos LM, Tetzloff G, Iyer SP, Maguire M, Golovko A, Zeng M, Wang L, Murgolo N, Graziano MP. Niemann-Pick C1 Like 1 protein is critical for intestinal cholesterol absorption. Science 2004;303:1201-1204.Peripheral tissues produce within cells all the cholesterol needed for cellular homeostasis. However, the liver is the only organ that is capable of degrading cholesterol. Therefore, cholesterol must be transported through blood to the liver for processing, degradation, and secretion into bile. Because cholesterol is an insoluble molecule, it must be packaged and transported by special particles in the plasma called lipoproteins. High-density lipoproteins (HDL) are responsible for movement of most cholesterol from peripheral tissues through the blood back to the liver. Because the liver is the center of cholesterol homeostasis in the body, cholesterol that moves from peripheral tissues to the liver is considered to be moving in the reverse direction.The balance of cholesterol in the body can be calculated from the enterohepatic circulation of bile salts as well as the movement of cholesterol from the liver into bile and the intake of dietary cholesterol. The average individual loses up to 1.2 g/day of cholesterol in the feces and 0.4 g/day of cholesterol as bile salts in the feces. This amounts to a total cholesterol loss of 1.6 g/day. The synthesis of cholesterol by the body equals the loss of cholesterol in the feces minus the dietary intake. Therefore, as shown here, the synthesis of cholesterol is up to 1.2 g/day, which exceeds the dietary intake by as much as 3-fold.Ezetimibe reduces cholesterol absorption. This decreases the content of cholesterol in chylomicrons. In the circulation, chylomicrons deliver triglycerides to muscle and fat tissue, but return to the liver with a full complement of cholesterol that was absorbed by the intestine. Therefore, ezetimibe reduces the flux of cholesterol from the intestine to the liver. Because this cholesterol is packaged and resecreted by the liver into the blood as VLDL particles, containing apo B-100, and because VLDL particles are the precursor particles of LDL in plasma, reduced flux of cholesterol to VLDL particles will lower LDL cholesterol. This mechanism is distinct from that of statins, which promote the clearance of LDL principally in the liver.Evidence that ezetimibe reduces LDL production may be inferred from a study in which patients with homozygous familial hypercholesterolemia were treated with ezetimibe plus statin therapy. The efficacy of statins is reduced in these individuals, in whom the LDL receptor is functionally absent. However, the efficacy of ezetimibe is largely unaffected. It is important to consider that ezetimibe therapy may lead to increased LDL receptor expression in individuals with functional LDL receptors, and that this may comprise a component of the mechanism by which ezetimibe lowers plasma LDL cholesterol and triglyceride concentrations.
Reference:Gagne C, Gaudet D, Bruckert E, for the Ezetimibe Study Group. Efficacy and safety of ezetimibe coadministered with atorvastatin or simvastatin in patients with homozygous familial hypercholesterolemia. Circulation 2002;105:2469-2475.