DUODENOSCOPY
Transcript of DUODENOSCOPY
1298
in dynamic and static 9 compliance in patients with acutepulmonary oedema. The analysis of Iff and Flenley there-fore does not seem very relevant to the cedematous situation.The second point arises from Flenley and Iff’s letter
(June 5, p. 1187) responding to some comments on theirarticle by Dr. Tattersfield and Dr. McNicol (May 1, p. 911).The point at issue is whether frusemide rapidly reduces theexcess extravascular water in acute pulmonary oedema. Iffand Flenley appear to misinterpret the measurements ofpulmonary extravascular water (P.E.v.) reported byMcCredie 10 and Kirk.ll Both these workers point outthat the double-indicator dilution technique measures
extravascular water in perfused parts of the lung only.There is direct 12 evidence and indirect 13 evidencethat the number of capillary channels open and perfusedis a function of pulmonary-artery pressure. Therefore the
higher the pulmonary-artery pressure, the greater themeasured P.E.v. A fall in pulmonary-artery pressureafter intravenous frusemide 14 may be associated with afall in measured P.E.v. but not necessarily a reduction inactual P.E.v. The issue cannot be resolved until P.E.v.
is measured in acute pulmonary oedema before and afterfrusemide. Even so, perfusion-dependent methods ofmeasuring P.E.v. must be interpreted with caution.
In acute pulmonary oedema, frusemide has no immediateeffect on blood-gases, minute volume, oxygen uptake (Iffand Flenley), dead-space tidal volume ratio, or percentagevenous admixture." Until new data become available, thesuggestion of Tattersfield and McNicol (May 1, p. 911) thatintravenous frusemide does not produce a rapid decreasein the amount of oedema in the lungs seems more plausible.
J. M. B. HUGHES.
Department of Medicine,Royal Postgraduate Medical School,
London W.12.
RELATIONSHIP AS A CLUE TO CAUSATION
D. P. M. HOWELLS.
Cardiff CF3 7DG.
(Formerly of M.R.C. TropicalResearch Laboratories,
The Gambia, West Africa.)
SIR,-Professor Osuntokun (March 27, p. 647) makessome valuable comments in connection with Mr. Burkitt’sarticle," and points out examples of reports which contra-dict some of the widely held views on the incidence ofcertain diseases in Africa. He states that the incidence of adisease in any population in developing countries dependson the availability and competence of medical staff, andurges that conclusions on the epidemiology of disease inthe African should be drawn with caution in the absenceof reliable field studies and adequate medical facilities.
There can be no doubt about the opportunity which ispresented, for the better understanding of the causationof disease by the contrasts in disease prevalence whichexist in different communities. But to define these differ-ences observations must be made on the prevalence andnot on the incidence of disease.
In 1968 the President of the Association of Surgeons ofWest Africa said " Gone are the days when impressions,dogmatic statements and generalisations were made aboutmedical conditions in West Africa ".11 If this statement is tobecome true of epidemiological studies in Africa carefulsampling of defined populations must be made. When the
9. Greene, D. G. in Handbook of Physiology: section 3, Respiration(edited by W. O. Fenn and H. Rahn); vol. n, chap. 70, p. 1595.Washington, 1965.
10. McCredie, M. Circulation, 1967, 36, 381.11. Kirk, B. W. J. appl. Physiol. 1969, 27, 607.12. Glazier, J. B., Hughes, J. M. B., Maloney, J. E., West, J. B. ibid.
1969, 26, 65.13. Permutt, S., Caldini, P., Maseri, A., Palmer, W. H., Sasamon, T.,
Zierler, K. in The Pulmonary Circulation and Interstitial Space(edited by A. P. Fishman and H. H. Hecht); p. 375. Chicago,1969.
14. Lal, S., Murtagh, J. G., Pollock, A. M., Fletcher, E., Binnion, P. F.Br. Heart J. 1969, 31, 711.
15. Tattersfield, A. E., McNicol, M. W. Clin. Sci. 1970, 38, 32P.16. Burkitt, D. P. Lancet, 1970, ii, 1237.17. Olu Williams, A. E. W. Afr. med. J. 1968, 17, 168.
characteristics of such populations are recorded it can thenbe decided what " natural experiments " and " experimentsof opportunity " exist to help elucidate the causation ofdisease.
DUODENOSCOPY
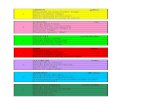
SIR,-We would agree with the conclusion of Dr. Shear-man and his colleagues (April 10, p. 726) that the Olympusduodenoscope represents a major advance in endoscopy.We were, however, disappointed firstly with the poorresults quoted and, secondly, that there was no descriptionof the techniques required for bulboscopy, since this is un-doubtedly one of the most important indications for
duodenoscopy.A failure rate of 8/15 patients with " definite radio-
logical evidence of duodenal ulceration is not only anunacceptable figure but also a misleading statement, sincethe radiological criteria are not defined. It is now becomingincreasingly clear that apparently obvious duodenal ulcersradiologically may on duodenoscopy show only a scarredbulb, and that non-agreement between radiology and bulb-oscopy may be as high as 40%.1,2
In a series of more than 100 duodenoscopies carried outin this department to date, we have found that the OlympusJF-B duodenoscope could not be passed through the
pylorus in less than 10% of cases as compared with the20% failure-rate quoted by Shearman et al. In addition,with the combined use of a forward viewing system(ACMI 7089-A) nearly 100% of the duodenal bulb can beexamined, the Olympus JF-B being especially useful forpyloric-canal lesions and an area just distal to the pyloricring. We cannot agree, therefore, with the conclusion ofShearman et al. that the JF-B may only have a limitedrole in the assessment of duodenal ulcers.Shearman et al. mention that cannulation of the ampulla
of Vater was not attempted in their series. We feel that thisprocedure is likely to be a major advantage of this endo-scope. The following case illustrates the value of thisprocedure.A woman aged 48 presented with a 3-week history of
Fig. 1.
1. Classen, M. in Carbenoxolone Sodium (edited by J. H. Baron andF. M. Sullivan); p. 157. London, 1970.
2. Salmon, P. R., Htut, T., Read, A. E. 3rd European GastrocameraSymposium. Berlin (in the press).
1299
Fig 2.
epigastric pain and back pain followed by jaundice. In-
vestigations revealed cholestatic jaundice (bilirubin 7-5 mg.per 100 ml., alkaline phosphatase 28 King-Armstrongunits, serum-aspartate-aminotransferase 250 units). A
straight radiograph of the abdomen was normal. Cholan-giography was not done because of the hyperbilirubinaemia.Duodenoscopy was performed under light sedation and theampulla of Vater visualised. The ampulla was cannulatedunder direct vision and contrast medium injected into thebiliary system, under screening control. With this pro-cedure a dilated biliary system was discovered with a
filling defect in the common bileduct near the ampulla(fig. 1) and multiple filling defects in a dilated cystic duct(fig. 2). Not only was one able to substantiate a diagnosisof gallstones but also additional information was providedsuggesting the presence of stones in the common bileduct.
P. R. SALMONP. BROWNT. HTUTR. BURWOODA. E. READ.
Departments of Medicine andRadiology,
University of Bristol.
BACTERIA ON ANTIBIOTIC TULLE
K. G. WESTCOMBE.
SIR,-We have been facing a mild epidemic of super-ficial infection in patients attending our hand clinic, andhave been trying to eliminate possible causes. At the timewe were using tins of antibiotic tulle. Following myinquiries into what were regarded as normal proceduresfor using this tulle, the following practices emerged:
1. Pieces of tulle were being removed from the tinand placed on the lid or put to one side for an indefiniteperiod. Tins were often incompletely closed.
2. Portions of tulle were being placed on the dressingtrolley and, if not used later, were being replaced in thetin.
3. At times, pieces were cut from the tulle squaresand the remainder replaced in the tin.
4. Attempts have been made by staff to have openedand partially used tins of tulle resterilised by normalhospital procedures. Were this to have succeeded theantibiotic would presumably have been inactivated.
Bacteriological studies on opened tins of more than onetype of tulle, which had been in use for one month or less,have shown that these tins do become contaminated withairborne organisms. The use of such tins can therefore beregarded as a breach in normal septic procedures. We havefound this breach can be effectively closed by the use ofindividually foil-packed and sterilised antibiotic tulle.
Individually packed items are certainly more expensive,but are probably less expensive in the long run than thetreatment of any resulting infection. Sources of infectionare always difficult to trace in hospitals, and anythingwhich will help to eliminate or diminish the human error,such as an individually packed dressing, is in my opinionworthy of consideration.Amersham,
Bucks. K. G. WESTCOMBE.
IgE AND THE NEPHROTIC SYNDROME
SIR,-We were particularly interested to note the findingsof Dr. Gerber and Professor Paronetto (May 29, p. 1097)regarding the presence of IgE in the glomeruli of patientswith the nephrotic syndrome. During the past eighteenmonths we have been studying three patients who have asteroid-sensitive nephrotic syndrome in association withgrass-pollen allergy and seasonal hayfever. The featurewhich is of particular interest to us is the annual relapse oftheir proteinuria, which occurs during the pollen season.Two of these patients remain in remission for most ofthe year; the third has persistent proteinuria which be-comes more severe in May and June.On one of these patients (a boy aged 13) we now have
serial estimations of a number of variables extendingover a full twelve-month period. With the help of Dr.S. G. 0. Johansson we have been able to study the variationin the serum level of IgE-both the total amount and thatspecifically reacting with grass-pollen. These measure-ments were made using the radio-immunosorbent assay(R.I.S.T.) and the radio-allergosorbent test (R.A.S.T.) respec-tively. 1., The total IgE levels are within the normal rangefor the large part of the year but rise quite steeply with theadvent of the pollen season. The level reaches a maximumof about five times the winter level and the peak coincideswith a similar peak in the grass-pollen-specific IgE level, theair-borne-pollen count, the 24-hour urinary protein excre-tion, hypoalbuminxmia, and the onset of oedema. This
patient is just commencing his fourth seasonal relapseand each has been readily sensitive to corticosteroid
therapy. There is no associated elevation of total
IgG, IgA, or IgM levels. Prick tests produce pro-nounced reactions to all grasses but none of the othercommon allergens. These results will be published in fullin the near future.Although a nephrotic syndrome in association with atopic
allergy has been described previously 3,4 we feel that it maybe more common than is at first apparent. Those patientswith a steroid-sensitive " minimal-change " nephroticsyndrome, who do not show a seasonal variation, may beproducing reaginic antibody against other allergens-e.g.,moulds, animal dander, dusts, or dietary factors. In viewof the importance of detecting atopic sensitivity in thesepatients it seems to us that skin-testing with a full range ofcommon allergens should be done in all patients with thiskind of nephrotic syndrome. Urine-testing of all patientswith atopic disorders should be carefully recorded andrepeated when they are in full relapse.
1. Johansson, S. G. O., Bennich, H., Wide, L. Immunology, 1968,14, 265.
2. Wide, L., Bennich, H., Johansson, S. G. O. Lancet, 1967, ii, 1105.3. Hardwicke, J., Soothill, J. F., Squire, J. R., Holti, G. ibid. 1959,
i, 500.4. Wittig, H. J., Goldman, A. S. ibid. 1970, i, 542.