Hemoragia digestiva superioara
-
Upload
denisa-oprisanescu -
Category
Documents
-
view
127 -
download
2
description
Transcript of Hemoragia digestiva superioara

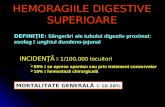
Hemoragiile digestive superioare
Clasificarea hemoragiilor digestive
Hemoragii digestive superioare (HDS) Sangerare de la nivelul esofagului pana la nivelul unghiului
Treitz(jonctiunea duodeno jejunala)*ligament Treitz-intre ultima parte a duodenului si ultima parte a stomacului.
Hemoragii digestive medii (HDM) Unghiul Treitz ® Valva ileocecala
Hemoragii digestive inferioare (HDI) Valva ileocecala ® Anus
Hemoragii digestive oculte(prezenta sangelui in scaun,dar fara a fi vazut cu ochiul liber)
Reactia Adler (1.5 – 2.5 ml sange in scaun)-reactia de culoare dintre Hb si apa oxigenata,pusa cu un reactive apoiculoare
Hemocult (> 5 ml sange in scaun) Hemoquant-cantitativ observa transformarea hemului nonfluorescent in
porfirina fluorescenta.Importanta HDS
Generalitati Frecventa - 1/ 2000 locuitori (UK)
Mortalitate 10 % (recent 4 %)
De 2 ori mai frecvente la varste > 60 ani
50 % prin ULCER è 1/ 3 AINS(antiinflamatoare nesteroidiene)
4 % prin VARICE è 1 / 3 DECES
De ce se produc sangerarile digestive?
1)Leziune mucozala inflamatorie injurie
2)Leziune vascularaDe 1 si 2 -Responsabil - tubul digestiv.
3)Deficit al hemostazei Factori de coagulare Trombocitele Vasele sangvine
4)Deficit al procesului de reparare al injuriei De 3 si 4 -Responsabil – ficatul.

Abordarea unei HDS
Diagnosticul pozitiv
Evaluarea gravitatii
Stabilirea efectelor hemodinamice
Diagnosticul etiologic
Tratamentul hemostatic
Etiologia HDS
Leziuni ale tubului digestiv Patologie esofagiana
o Hemoragie esofagiana – explozie sau eroziune (85%) – sunt hemoragii medii sau severe
o Esofagita de reflux – sunt hemoragii usoareo Hernie gastrica transhiatalao Ulcere esofagieneo Cancere esofagieneo Tumori benigne esofagiene
Patologie gastricao Ulcer gastric
Mica curbura, unghi gastric, sub cardial Prepiloric, fata anterioara ® 30% sunt severe
o Gastrita eroziva Stress chirurgical, arsuri intinse Medicamente (AINS) HDS moderate
o Cancer gastric operat – HDS moderateo Polipi/polipoze – HDS usoareo Cauze rare
Angiodisplazia gastrica (malformatii vasculare) Sd. Mallory-Weiss (alcool + varsaturi)
o Stomac operat Sutura / ulcer / cancer gastric
Patologie duodenalao Ulcere duodenale mai ales de fata posterioara – sangerari moderate
sau severe (70%)o Duodenita acuta + gastrita acuta hemoragicao Tumori duodenale – raro Cauze rare
Varice duodenale Pancreas ectopic

Leziuni la nivelul glandelor anexe Patologie hepatica
o Hipertensiune portalao Hemobilia
singe la nivelul cailor biliare manifestat prin triada COLICA + MELENA + ICTER
Origine – ficat / vezicula biliara / cai biliare / pancreas Patologie pancreatica
o Cauze “benigne” ® PAC, PCR?o Cancere pancreatice invaziveo HTP segmentara
Cauze extradigestive
Sindroame hemoragipare prin:
Coagulopatii
Purpure
Hemofilie
CLINICA Hemoragia
Exteriorizare Hematemeza Melena Hematochezie Oculte
Consecinta Hematologica Hemodinamica
Cauza
Paraclinic EDS
Forrest I = Activa
a. jet pulsatil / nepulsatil b. panza
II = Stigmate a . Cheag b . Vas
III = potentiale HDS
AOB

Hb, Ht, L Uree FOBT Rx Arterio Hematii marcate *
BOALA DE BAZA Ciroa Hemopatii Coagulopatii
Gravitate (Smith & Weil)
Usoare = 25%1250 ml
AV = 100b/minTA = 90 mmHgIS <1?PVC =ND (diureza)= N
Medii = 35 %1750 ml
AV = 120TA= 90IS <1,5PVC scadeD scade
Severe = 50 %2500 ml
AV > 120TA < 60IS > 1,5PVC F. scazutaANURIE =soc !
TIMP !!!
Atitudinea terapeutica in HDS Conditii necesare
Personal medical calificat / interdisciplinaritate: gastroenterolog, endoscopist, anestezist, chirurg, asitent medical
Camera de garda – dotare ATI adecvata

Posibilitate de a institui transfuzii sangvine Laborator aceesibil 24 ore din 24 Posibilitatea de a efectua EDS 24 h din 24 Existenta unor protocoale de inteventie si monitorizare a bolnavilor Accesul la serviciul de chirurgie
Protocol HDS Diagnostic pozitiv – hematemeza + melena – TR + sonda
Da Nu ® acasa
Evaluarea gravitatii Usoara / Medie + pacient < 60 ani, Hb>10, TA (N)
Sectie boli interne sau gastroenterologie, EDS ® 5 zile Grava + pacient > 60 ani, Hb < 10, hipovolemie, boli asociate
ATI, PEV?, chirurgie Se determina: Hb, uree, grup sg., coagulograma, teste hepatice
Rechilibrare hidroelectrolitica Detectarea sursei de sangerare Selectarea tipului de tratament :
Medical Endoscopic Interventional (TIPS)- Transjugular Intrahepatic Portosystemic Shunt
(TIPS)?*
Chirugical*TIPSInterventional radiologists perform this procedure to treat a condition called portal hypertension. Portal hypertension occurs most frequently in patients with liver disease such as cirrhosis or hepatitis. Scarring in the liver creates a restriction to the flow of blood through the liver. The main vein to the liver is the portal vein. The pressure in the portal vein becomes very high, causing adjacent veins in the abdomen to become dilated (varices) and can potentially rupture and cause life-threatening internal bleeding. By lowering the pressure in the portal vein, the risk of hemorrhage is greatly reduced.
The TIPS procedure has also been effective in the treatment of ascites secondary to liver disease. In addition, TIPS has been successfully applied in less common situations including treatment of Budd-Chiari syndrome, decompression of lower GI and stomal varices, and treatment of malignant compression of hepatic or portal veins. This procedure is a good alternative to the surgical treatment of this condition with a shorter recovery time.
The initial TIPS procedure is performed under general anesthesia. The interventional radiologist threads a thin catheter (tube) through a small incision in the neck and guides it to the blood vessels in the liver. Under x-ray guidance a connection between the inflow vein of the liver (portal vein) and the outflow vein of the liver (hepatic vein) is made to divert the flow of blood and decompress the portal vein. The connection is held open by an expandable metal tube that remains inside the liver.
You may be admitted to the hospital before or directly after the procedure and can potentially be discharged the following day. Within the first year routine follow-up at 3 month intervals is necessary to assure that the shunts remain open and adequately functioning. Revisions of the shunt are

performed in a similar manner to the original TIPS procedure but are typically performed as an outpatient.
Pre-procedure Information Your doctor will schedule you for a pre-procedure evaluation by the Vascular & Interventional Radiology (VIR) service. Report to Diagnostic Imaging-D (3rd floor, Green Zone) for your scheduled appointment. The procedure will be performed on a subsequent day. They will discuss the planned procedure with you and answer any questions you may have about the procedure, its risks and benefits. Please inform us if you are diabetic, pregnant, or allergic to contrast media ("dye"). We will also need to know if you have a history of heart disease or have respiratory problems.
If additional laboratory or imaging studies are needed prior to your scheduled procedure they will be arranged during this visit. Bring any outside films (x-rays) with you, if you have not already given them to your physician. Pre-procedural patient work-up and preparation includes visualization of hepatic arterial and venous structures as well as assessing patency of the portal venous system. This is most commonly performed with Doppler ultrasound but can also be assessed with magnetic resonance venography. It is critical to aggressively correct a patient’s coagulopathy with vitamin K, fresh frozen plasma, and if necessary, platelets given the high risk of intraperitoneal bleeding. In addition, patients receive broad spectrum antibiotic coverage.
Please call (713) 794-1180 (during working hours) if you are unable to keep your appointment.
Important Instructions
You must be accompanied by a responsible adult following your procedure Do not eat or drink for a minimum of 6 hours prior to your procedure You may take your daily medications with sips of water
Discharge Instructions Rest at home and avoid strenuous activities for for a minimum of 24 hours. You should also contact your doctor if you have a fever of 101 degrees Fahrenheit (38.3 degrees Celsius) or higher, or if you have redness, swelling, bleeding or drainage from the site where the catheter was inserted.
Please call Diagnostic Imaging-D at (713) 794-1180 (during working hours) or the M.D. Anderson Emergency Center at (713) 792-3722 (24 hours a day).
Tratament medical in HDS
I. Combaterea efectelor hemodinamice
II. Substante vasoactive
III. Tratament hemostatic temporar - EDS T
IV. Tratament hemostatic definitiv
Combaterea efectelor hemodinamiceIMEDIAT CACI IMPREVIZIBILNU SANGEE CACI MICROCIRCULATIE

MOMENT REVERSIBIL
Scade volemiascade debit incetinire circulatieScade volemia Scade vascozitatea creste hematocrit capilar = ORT
MOMENT IREVERSIBIL
Dezoxigenare eritrocit rigidizare ORDRigidizareAgregare plachetara CID
Modalitate Inlocuire volemica = solutii cristaloide Sange si O2 hiperbara Volum
PVC TA AV
Substante vasoactive Doar in soc Doar la pacientul cu inlocuire volemica Doar scurt timp
Dopamina, DobutaminaTratament hemostatic “temporar” = endoscopic
Variceala Ligatura Scleroterapie clips-uri
Nonvariceala Injectare Electrocauterizare Laser Argon plasma
HDS non - varicealaTratamentul HDS nonvariceala
Gastrite, duodenite, sindroame hemoragipare – tratament medical Sindromul Mallory Weiss – injectare de alcool Ulcer gastric, cancer gastric – trat. chirurgical Ulcer duodenal
< 40 ani la prima sangerare – trat. medical a doua sangerare – trat. chirurgical
> 40 ani, recidiva la 48 ore – trat. chirurgical

HDS varicealaTratament HDS variceala
Varice Tratament HDSTratament HTPTratament EPH?
Tipul de interventie in HDS variceale Profilaxia primei sangerari
EDS Trat HTP Antisecretor
Profilaxia resangerarii Tratamnetul HTP Antisecretor
Tratamentul HDS variceale acute Medical (octreotid/vapreotid, antisecretor manevre locale (sonda) endoscopic radiologie interventionala (TIPPS)-trans illuminated powered
phlebectomy surgery) chirurgical
*Procedure At A Glance TIPPS Procedure is intended to reduce varicose and spider veins, and resurface the skin on the legs by improving blood vessels. This procedure is likely to be expensive and possibly painful, and also requires a significant amount of time for an individual to heal. We’ll take a closer look.
Procedure In Focus TIPPS Procedure is a surgery that requires an incision, during which doctors distribute saline solution and insert a suction device to remove problematic veins. During TIPPS Procedure, doctors remove abnormal veins, allowing those that are functioning more blood flow. However, with some of the amazing products available on the market today, we feel TIPPS Procedure seems unnecessary for most. With top quality products that include ingredients like Diosmin 95®, many people are finding that they may achieve amazing skin care without having to schedule appointments or undergo surgical procedures.
When searching for a skin care formula, we strongly believe people should always look for Diosmin 95®. Diosmin 95® is an ingredient that was recently made available over the counter, and has shown amazing results for addressing varicosity. This ingredient has been clinically proven to repair blood vessels and rebuild damaged skin areas. When

searching for a skin care product, we think it is crucial for individuals to look for this ingredient.Positives • Minimally invasive surgery • Said to reduce varicosity• Claimed to remove broken veins
Negatives • Doesn’t use Diosmin 95®• Rather high cost• Requires time to heal• No refund policy or customer service
Cost
10,000 - 35,000 $ / EPISOD HDS VARICEALA Sharara A, Rockey D - New Engl J Med, 2001; 345; 669 - 81
Concluzii
1. HDS reprezinta inca o cauza importanta de morbiditate si mortalitate la populatia adulta.
2. Modalitatile terapeutice sunt diferite in HDS variceale si non-variceale. 3. Terapia endoscopica a produs modificari majore in mortalitatea prin HDS
indiferent de cauza; tratamentul antisecretor reprezinta una din cele mai importante solutii adjuvante ale terapiei endoscopice.
Hemoragie obscura-apare in scaun dar nu se cunoaste cauza ?