Conferința Societății Naționale de Oncologie Medicală din...
Transcript of Conferința Societății Naționale de Oncologie Medicală din...

Revista Hipocrate România Octombrie 2012
Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România Hipocrate iPadRevista este acum la degetul tău. La propriu
Ediția a XI-aPoiana, Brașov, 11-14 octombrie 2012
Rezumatele lucrărilor
Conferința Societății Naționale de Oncologie Medicală din România

Colecţia de
primăvară
2012
Publicaţie trimestrială pentru sănătatea ta
și a familiei tale
Revista 4P
Învingem cancerul!
O dată-n viaţă
Sănătatea copilului:Sănătatea copilului:
Cum luptăm cu efectele adverse
ale chimioterapiei?
O lecție de autoapărare: vaccinarea
Tulburările de creștere și dezvoltare
Sănătatea adultului:Sănătatea adultului:
Jurnalul unui supraviețuitor de infarct
Să rupem tăcerea din jurul prostatei
Osteoporoza: boala care te fură pe neștiute
Legături periculoase între inimă și creier:
fibrilația atrială și accidentul vascular cerebral
Util: Cele mai active asociaţii ale pacienţilor din România
Povesteamea
Sănătatea vârstei a treia:
Sănătatea vârstei a treia:Iuliana Tudor
Pret: 6,9 RON
Rev
ista
4p
- P
erso
nal
izar
e P
reve
nți
e Pa
rtic
ipar
e P
red
icți
e

Rezumatele lucrărilor

| Septembrie 20124
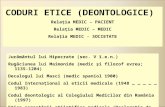
l Prof. Dr. Florin B`dulescu1, Dr. Marius Geant`2, dr. Michael Schenker
1 Profesor de oncologie medical`, pre[edinte al Societ`]ii Na]ionale de Oncologie Medical` din România
2 National Task Force Romania al Public Health Genomics Network Europe
În ciuda faptului c`, în ultimele decade, au fost ob]i nute succese semnificative în ceea ce prive[te s`n`tatea uman`, progresele înregistrate au fost neuniforme. Diferen]ele se p`streaz` atât între zonele geografice, cât [i între ariile terapeutice. Nu to]i pacien]ii r`spund la cele mai folosite medicamente, iar în rândul celor care r`spund pot exista reac]ii adverse adesea severe, care fac imposibil` continuarea tratamentului. Un procent estimat de 57% din totalul intern`rilor în spital este din cauza reac]iilor medicamentoase adverse, în timp ce o cincime dintre decese apar ca urmare a efectelor adverse ale terapiilor.
90% dintre medicamentele folosite acum sunt eficiente la numai 40% dintre pacien]i. În timp ce, în prezent, majoritatea pacien]ilor primesc medicamentele mai mult sau mai pu]in în acela[i mod, tratamentul în viitorul nu prea îndep`rtat va fi ajustat la grupurile de pacien]i selecta]i, defini]i prin propriile semn`turi moleculare. Aceasta este ceea ce definim drept medicin` personalizat`, sau utilizarea aspectelor moleculare [i a testelor diagnostice pentru a ajusta mai bine administrarea medicamentelor [i pentru a gestiona în mod superior boala unui pacient.
Provoc`rile medicinei personalizateMedicina personalizat` implic` numeroase
provoc`ri. Odat` cu maparea genomului uman, au fost ob]inute o multitudine de informa]ii privitoare la modul
în care oamenii difer` unul fa]` de cel`lalt [i la modul în care structura genetic` individual` poate influen]a susceptibilitatea unei persoane pentru o boal` [i r`spunsul la noile tratamente. Genomica nu este singura dintre noile discipline, denumite generic „omice“, care încearc` s` defineasc` [i s` explice mecanismele corpului uman. Proteomica, sau studiul pe scar` larg` al proteinelor, este o alt` astfel de disciplin`. Exist`, de asemenea, epigenomica, transcriptomica, metabolomica [i metagenomica.
Principala cauz` a e[ecurilor studiilor clinice de faza II [i III nu este reprezentat` de siguran]a sau de profilul de toxicitate al medicamentului, ci de eficacitatea acestuia. Acest deficit al dezvolt`rii medicamentelor noi poate fi explicat printro în]elegere insuficient` a mecanismului apari]iei bolii la nivelul fiec`rui pacient. Cu alte cuvinte, dac` nu [tim ce se întâmpl` cu adev`rat la nivelul pacientului individual, [ansele de al trata cu succes sunt foarte mici.
Medicina modern` a oferit suficient de multe informa]ii despre entit`]i patologice individuale, dar în acest moment cunoa[tem destul de pu]ine lucruri despre conexiunile dintre acestea. Bolile reprezint` o re]ea complex`, în ochiurile c`reia se afl` componente moleculare, celulare [i fiziologice, toate acestea alc`tuind sistemul biologic uman, unic pentru fiecare individ. De aceea, esen]ial este s` privim în ansamblu, nu doar izolat, o boal`, un tratament [i efectele acestuia, pentru fiecare pacient care ne intr` în cabinet.
Rolul tehnologiei informa]iei [i comunica]iilor
Sub umbrela medicinei personalizate, se dezvolt` din ce în ce mai multe tehnologii care s` ajute la oferi
În loc de introducere
Medicina viitorului începe de ast`zi. Cu medicina
personalizat`, în oncologie
www.revista-hipocrate.ro REZUMAT

Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România
Septembrie 2012 | 5
rea unui tratament individualizat. Cum genomul pare a fi elementul cheie în acest demers, studii recente au ar`tat c` pot fi combinate diverse profile genomice întrun profil integrativ personal, individual, pentru a monitoriza schimb`rile survenite în c`ile biologice, atât la persoana s`n`toas`, cât [i la cea bolnav`, cu scopul de a evalua riscul medical.
Utilizând tehnologia informa]iei [i a comunica]iilor pentru a sus]ine integrarea la scar` larg` a informa]iei, este posibil, întrun viitor nu prea îndep`rtat, s` avem acces la o în]elegere la nivel de sistem a s`n`t`]ii fiec`rui om, o abordare care acum lipse[te în multe arii terapeutice [i, în final, s` identific`m solu]iile de asisten]` medical` personalizat`.
Demersul reprezint` o provocare major` nu doar pentru cercetarea medical`, ci [i pentru industria IT, care trebuie s` identifice solu]ii pentru stocarea unui volum uria[ de date. De exemplu, pentru a integra informa]ia con]inut` în corpul unui singur individ, cu mijloacele cunoscute la acest moment, este necesar` o energie de 100.000 de ori mai mare decât cea generat` de Soare!
Fenomenul de îmb`trânire a popula]iei [i presiunea asupra bugetelor
Demografia joac`, de asemenea, un rol din ce în ce mai important în contextul social actual [i din viitorul apropiat. Persoanele vârstnice constituie o propor]ie din ce în ce mai mare din popula]ie, iar costul asisten]ei medicale este în cre[tere, punând în discu]ie sustenabilitatea pe termen lung a sistemului de asigur`ri de s`n`tate.
Cheltuielile în sistemele de s`n`tate sunt din ce în ce mai mari. Omenirea sa bucurat de un succes enorm în prezent existând aproximativ 7.500 de medicamente disponibile pentru pacien]i în întreaga lume – [i totu[i acest succes este o barier` în calea progresului. Vor exista foarte pu]ine medicamente noi pân` când vom putea în]elege mai bine cum putem reclasifica bolile la nivel molecular.
Educarea medicilor [i a pacien]ilor în direc]ia personaliz`rii
O alt` problem` important` o constituie instruirea medicilor [i informarea pacien]ilor. Medicii vor trebui instrui]i întrun num`r de discipline, pentru a în]elege [i a putea utiliza toate instumentele sofisticate pe care le vor avea la dispozi]ie pentru medicamentele personalizate. Odat` instrui]i, ace[tia vor trebui s` aib` acces la facilit`]ile de diagnostic [i de tratament, pentru a asigura aceast` asisten]` în conformitate cu principiul UE al egalit`]ii accesului la sistemele de s`n`tate [i cu cel al accesului universal la medicamente.
Modul în care este practicat` meseria de medic se afl` întro transformare rapid`. Timp de mii de ani, diagnosticul [i tratamentul sau bazat pe ceea ce se putea vedea, mirosi, gusta [i intui. În ultimii 100 de ani, diagnosticul a evoluat, ajungând s` includ` cuno[tin]e ale proceselor biochimice [i celulare. În prezent, diagnosticul [i tratamentul includ elemente de biologie molecular` [i de genetic`. În viitor, managementul pacien]ilor va trebui s` se bazeze pe analiza computerizat` a informa]iilor moleculare pentru a
identifica tratamentele optime sau necesare pentru pacien]i, la nivel individual.
Un model pentru autorit`]iOferind pacien]ilor medicamente personalizate, furni
zorii de asisten]` de s`n`tate pot evita încerc`rile [i erorile [i pot reduce reac]iile adverse. Aceasta asigur` un poten ]ial de beneficii majore pentru pacien]i [i pentru sistemul sanitar ca întreg. În prezent, acest poten]ial este în mare m`sur` neexploatat. De exemplu, 640 de milioane de euro sar economisi anual, la nivel mondial, prin introducerea test`rii pentru mutat]ia KRAS în cancerul de colon, urmat` de instituirea unui tratament t]intit.
Autorit`]ile franceze au instituit un program na]ional pentru pacien]ii cu cancer, în cadrul c`ruia ace[tia pot fi testa]i, gratuit, în privin]a caracteristicilor moleculare ale tumorilor lor. Aceste teste sunt efectuate în oricare dintre cele 28 de centre regionale. Odat` testa]i, pacien]ilor li se pot prescrie cele mai adecvate medicamente, imediat ce acest lucru este posibil. Programul a fost ini]iat în 2006, ca r`spuns la cererea pacien]ilor de acces la cele mai noi terapii ]intite pentru cancer. Programul este derulat de c`tre Institutul Na]ional pentru Cancer (Institut National du Cancer) [i de c`tre Ministerul S`n`t`]ii. Laboratoarele din cele 28 de centre regionale administreaz` teste, pe baza c`rora mostrele tumorilor pacien]ilor sunt analizate, iar cancerele definite. Abordarea privitoare la clasificarea tumorilor sa modificat, odat` cu introducerea diagnosticelor moleculare; se cunoa[te acum, de exemplu, c` tumorile maligne colorectale constau din cel pu]in patru subseturi patologice, fiecare corespunzând unei anumite muta]ii genetice. La fel se întâmpl` [i în cazul cancerului pulmonar f`r` celule mici, care poate fi caracterizat de [apte muta]ii diferite sau transloca]ii cromozomiale.
De la “evidence based medicine” la “value based medicine”
În concluzie, anii care urmeaz` vor consemna transla]ia de la prescript]ie la prevent]ie, de la pacientul mediu la pacientul individual, de la abordarea reduct]ionista` a dezvolta`rii medicamentelor la o abordare care prives]te boala în ansamblu, nu doar un fragment, de la sistemul centrat pe medic la sistemul centrat pe pacient. [i, nu în ultimul rând, de la “evidence based medicine” la “value based medicine”. Iar oncologia se afl` în avangarda acestei revolu]ii care a început în medicin`.
România: unde suntem [i unde putem ajunge?Pentru România, însu[irea profund` a principiilor me
dicinei personalizate poate reprezenta o cale scurt` pentru recuperarea decalajelor care ne separ` de statele occidentale. Dup` ani de zile în care reforma ghidurilor de practic` pe modelul vestic în oncologie a fost blocat`, ca [i constituirea Registrului Na]ional de Cancer, în anul în care criza oncologicelor ieftine a ]inut prima pagin` a massmediei, a discuta despre medicina personalizat` reprezint` o sacr` obliga]ie, nicidecum o curiozitate. Ea deriv` din principiul fundamental al lui Hipocrate, p`rintele medicinei: “Primum non noncere (în primul rând, s` nu faci r`u)”.

| Septembrie 20126
l Dr. G. Ionescu, Dr. C. Mazilu, Dr. C. Stan, Fiz. C. PopescuPETCT Department Euromedic Fundeni
FDG PETCT is an important imaging tool in the noninvasive evaluation and monitoring of children with known or suspected malignant diseases. In this presentation, we discuss the preparation of children undergoing PET studies and review radiation dosimetry and its implications for family and caregivers, normal 18FFDG distribution in children, and various artifacts that may arise.
We explore the use of FDGPET in the study of children with the more common malignancies, such as brain neoplasms and lymphomas, and the lesscommon tumors, including neuroblastomas, bone and softtissue sarcomas, Wilms’ tumors, hepatoblastomas and germcell tumors.
We will also present the limits and the absolute and relative contraindications of 18FFDG PETCT assessment of oncologic disease in children, including main causes of falsepositive and falsenegative results.
General considerations in patient preparation and radiation dosimetry will be discussed.
PETCT Imaging in Oncopediatry Advantages and Limits
www.revista-hipocrate.ro REZUMAT
l Dr. C. Mazilu, Dr. G. Ionescu, Dr. C. Stan, Fiz. C. Popescu
PETCT Department Euromedic Fundeni
PurposeWe tried to analyze characteristics and amount of
18FFDG uptake in soft tissue and bone tumors and investigated the ability of 18FFDGPET/CT to differentiate malignant from benign tumors; also we tried to investigate the advantages and limits of FDG PETCT in local and systemic assessment of musculoskeletal tumors.
Material and MethodWe included 39 patients, from June 10 to June 2012,
who performed PETCT for assessment of local or systemic disease. The final diagnosis was obtained from surgical biopsy or clinical followup. We analyzed the characteristics and amount of 18FFDG uptake in soft tissue and bone tumors and ability of 18FFDGPET/CT to diffe
rentiate malignant from benign tumors, using maximum standardized uptake value (SUVmax).
ResultsFinal diagnosis revealed 3 benign soft tissue tu
mors (mean SUVmax 4.7), 2 benign bone tumors (5.1), 19 malignant soft tissue tumors (8.8), and 15 malignant bone tumors (10.8). There was a significant difference in SUVmax between benign and malignant musculoskeletal tumors in total, soft tissue tumors and bone tumors.
ConclusionsFDGPET/CT allows delineation between malignant
and benign soft tissue and bone tumors, although there were many falsepositive and false negative lesions. Further studies with all kinds of musculoskeletal tumors in large numbers are needed to improve the diagnostic accuracy of 18FFDGPET/CT.
Fusion Imaging Assessment of MusculoSkeletal Tumoral Pathology
Detecting Mutations in the EGFR Gene in NSCLC in Order to Guide Personalized Therapy with TyrosineKinase Inhibitors
l Georgeta Cardos1, Andi Palade1, Alina Geor-gescu1, Mihai Stoicea1, Diana Teletin1, Bogdanka Mi-litescu1, Gra]iela Tardei1,2
1„Personal Genetics” Medical Genetics Center, Bucharest, Romania
2„Dr. Victor Babe[” Hospital, Bucharest, Romania
The EGFR gene codifies the Epidermal Growth Factor Receptor, which is a transmembrane protein with tirosinekinase activity, involved in cell growth and differentiation. Somatic mutations in exons 1821 of the EGFR gene, identified in 1030% of nonAsian patients with non–smallcell lung carcinomas (NCSLC), trigger consti

Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România
Reclama

| Septembrie 20128
tutive activation of the EGFR receptor and play a crucial role in tumor progression. EGFR mutational status is a predictor of benefit for EGFRTKI (tyrosine kinase inhibitors) therapy.
The aim of our study was to detect the EGFR mutational status in exons 19 and 21 (cca 90% from all mutations) in lung adenocarcinoma patients, in order to contribute to selection of patients for the new EGFRTKI personalized therapy.
DNA was extracted from fixed and paraffin embedded tumors from 87 lung adenocarcinoma patients and EGFR mutational status analyzed by ARMSPCR and sequencing.
Activating mutations were detected in exons 19 and 21 of the EGFR gene in 19 tumors out of the 87 analyzed (21,84%), of which 15 tumors with deletions in exon 19 and 4 tumors with point mutations in exon 21; the amount of tumor cells was variable, between 90% and 5%. The 19
patients were aged between 47 and 85 year, and sex distribution was 1,1:1 (F:M); 15 of t h e m were nonsmokers.
Our results have confirmed the sensitivity and cost effectiveness of our molecular methods in testing of the EGFR mutational status, contributing to an effective selection of patients with NSCLC for antiEGFR personalized therapy.
www.revista-hipocrate.ro REZUMAT
An Observational Study to Assess the Safety and Efficacy of Eligard 7.5 mg and 22.5 mg for the
Treatment of Advanced Prostate Cancerl St`nculeanu D. L.1, Ullmann F.2. Sefchi C.3 1Prof. Dr. Alexandru Trestioreanu Oncology Clinical Institute, Bucharest, Romania 2Astellas Pharma International B. V., Medical Department, Leiderdorp, The Netherlands 3Astellas Pharma S.R.L., Medical Department, Bucharest, Romania
Introduction and ObjectivesDespite the effectiveness of orchiectomy to treat pros
tate cancer, treatment with LHRH agonists is often preferred my physicians and patients. This observational study was conducted in 12 oncology centers in Romania, between February 2009 and Decenber 2010, assessing the safety, efficacy and handling of two formulations of Eligard (Astellas Pharma).
Materials and MethodsIn this noninterventional survey with a duration of 12
months, Eligard 7.5 mg (1 month depot formulation) or 22.5 mg (3 months depot formulation) were administered to 120 patients with advanced hormonedependent prostate cancer. The study was conducted in the setting of routine outpatient medical care. Data were collected after 6 and 12 months of treatment and were analyzed descriptively.
ResultsEfficacy. Median PSA concentration at baseline was
9.1 (range 0.07460) ng/mL, decreasing to 0.7 (0.0174.8) at 6 months and 0.4 (0.001397.5) at 12 months. Median testosterone concentration decreased from 5.3 (0.1862) ng/dL at baseline to 0.2 (0.128.3) at month 6 and 0.2 (0.158.6)
at month 12 (data available for 11 patients). Only a small number of patients discontinued the drug because of an inadequate response to treatment (4 of 120; 3.4%). Clinicians indicated that their primary reason for prescribing Eligard was its efficacy profile (89 of 165 reasons given).
Safety. Nine patients died from causes related to their primary diagnosis of cancer. Two patients experienced an adverse event which was not related to study drug. The number of tolerability issues and the nonserious adverse events were lower than the ones reported in the registration studies and in the literature.
ConclusionsIn this Romanian observational study, Eligard 7.5 mg
and 22.5 mg were demonstrated as both efficacious and tolerable. Testosterone levels were reduced and maintained during the 12 months study period and PSA concentrations were brought be l o w normal levels at months 6 and 12. Healthcare professionals identified the handling and administration of the Eligard syringe as practical. The data of this outpatient Romanian observational study was consistent with that of the Eligard registration studies.

Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România
Reclama

| Septembrie 201210
Management of mCRPC Patients – A Closer Look at New Therapeutic Alternatives
l Anca Mihailov MDmCRPC patient population is highly heterogeneo
us. Until recently, treatment of advanced prostate cancer was only palliative and once resistance to hormonal therapy had developed – so called ‘castration resistant prostate cancer’ (CRPC), median life expectancy did not exceed one year. The paradigm changed in 2004 when two large studies demonstrated, for the first time, a survival benefit with docetaxel. In June 2010 Jevtana was approved by the US Food and Drug Administration (FDA) and by European Medicine Agency (EMA) in 2011 for the treatment of patients with hormonerefractory metastatic prostate cancer who had been previously treated with a regimen con
taining the taxane docetaxel.In TROPIC study, cabazitaxel treatment significantly
improved overall survival response in patients previously treated with docetaxel more than twofold compared with mitoxantrone, the probability of surviving at 2 years with cabazitaxel (28%) being much higher than with mitoxantrone (17%). Also, cabazitaxel doubled median PFS compared with mitoxantrone (cabazitaxel 2.8 months vs mitoxantrone 1.4 months; p<0.0001), the PSA response rate was significantly higher in the cabazitaxel group and, also, the patients had a significantly longer time to PSA progression. The updated analysis data highlighted the benefit of cabazitaxel over mitoxantrone across multiple patient subgroups.
www.revista-hipocrate.ro REZUMAT
l Dr. Dana St`nculeanu Institutul Oncologic „Prof. Dr. Al. Trestioreanu“ Bucure[ti
TAM therapy of ER+ breast cancer distant metastases compose the majority of early recurrences during TAM therapy (~75% of all early recurrences are distant metastases)(1, 2).
Adjuvant treatment strategies include:Upfront (early adjuvant at start);Sequencing;Switching;Extended adjuvant.Adjuvant regimens are presented: trial designs, pati
ent characteristic, results(4, 5, 6).
BIG 1-98(3, 8, 9)Letrozole significantly reduced early distant me
tastasis (initial 26 months followup data);The superiority of LET in the primary core analysis
led to the unblinding of the TAM monotherapy arm> ITT analysis may have a potential bias against LET/ censored analysis potential bias against TAM (for survival, recurrence events)> a weighted analysis was necessary.
Inverse probability of censoring weighted IPCW analysis(8, 9):
Weights the followup for the women who stay on TAM to account for the censored followup of matched patients who crossover;
A validated methodology used in several clinical trials.
BIG 198 sequential and monotherapy updates at 8.1 years: IPCW analyses on DFS, OS, DRFI, BCFI confirms LET superiority over TAM(8, 9).
Other 8.1 years updates from BIG 198(9, 10) are:
Early LET treatment may be beneficial for patients with nodepositive disease;
Patients at greatest risk for early recurrence had: tumors ≥ 5 cm, grade 3 tumors, ER+/PgR– tumors, ≥ 4 positive nodes, vascular invasion.
Future directions include:Assess potential strategies to counter acquired en
docrine resistance;Identification of most effective AI for adjuvant the
rapy;Maximizing benefit from endocrine treatment.
Summary1. Adapted from Mansell J, et al. Breast Cancer Res Treat. 2009;117(1):9198; 2. Baum M, et al. Lancet. 2002;359(9324):21312139; 3. Thürlimann B, et al. N Engl J Med. 2005;353(26):27472757. 4.Dowsett M, et al. J Clin Oncol. 2010;28(3):509518; 5. Ingle JN, et al. Ann Oncol. 2008;19(5):877882; 6. Jakesz R, et al. J Natl Cancer Inst. 2007;99(24):18451853. 7. Mauriac L, et al. Ann Oncol. 2007;18(5):859867. 8. Colleoni M, et al. JCO. 2011;29(9):11171124 . 9. Regan M et al: Lancet Oncol 2011; 12: 1101–08; 10. Viale G, et al. Ann Oncol. 2011; 22: 2201–2207
BIG 198 Trial Clinical Impact and Recent Updates

Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România
Reclama

| Septembrie 201212
Bevacizumab in Her2Negative Metastatic Breast Cancer Patients, from Clinical Trials to Clinical
Practice Results of Petra NonInterventional Studyl Dr. Dana Lucia St`nculeanu Bucharest Oncology Institute, Medical Oncology Department
BackgroundAdvances in the treatment of earlystage breast cancer
have improved outcomes for patients. Despite these improvements, however, many women ultimately develop metastatic breast cancer (MBC). MBC is essentially an incurable disease, and the prognosis has changed little over the past decade. Avastin in combination with paclitaxel or capecitabine have proven to be effective in improving outcomes in HER2 negative metastatic breast cancer patients in E2100 and RIBBON 1 studies. This is a prospective, multicenter, observational, noninterventional cohort study, in subjects with HER2 negative metastatic breast cancer receiving therapy with Avastin. The study was sponsored by Roche Romania SRL
Study Rationale and ObjectivesThe rationale of the present noninterventional study
was to collect information from real world daily clinical practice on efficacy and safety of Avastin treatment. The primary objectives were the incidence of serious adverse events related to bevacizumab and the incidence of specific adverse events (serious and nonserious). The secondary objective was to assess the efficacy of bevacizumab, as measured by time to disease progression and duration of survival.
Patients and MethodBetween 2007 and 2010, 36 patients treated with Avas
tin for their HER2 negative metastatic breast cancer, according to standard of care and in line with local labeling and local guidelines, were followed for safety and efficacy for the duration of their treatment with Avastin. The medi
an age was 49 (range 2669). 34 (94.45%) patients had an ECOG PS of 0 and 1 at baseline; 6 (17%) patients had hormonal receptor status negative at baseline. 24 (67%) had one metastatic lesion, 10 (28%) had two metastatic lesions and 2 (5%) had 3 or more metastatic lesions at baseline.
ResultsAvastin was combined with taxanebased therapy
in 89% of patients. The median duration of therapy with Avastin was 45,5 weeks (range 3–124 weeks). The median number of visits was 22 (range 263). 21 (58%) patients didn’t experience variation on blood pressure. 10 (28%) patients had an increase of blood pressure < 20 mmHg and one patient had an increase on blood pressure >20 mmHg. Only 2 (6%) patients had proteinuria 1+.
Other adverse events reported during Avastin therapy were: minor hemorrhage (2 patients), handfoot syndrome (1 patient) and diarrhea (1 patient). There were no statistically significant variations in treatment tolerability, ECOG PS and body weight, between first and last Avastin treatment visits. The median time to disease progression was 79 weeks (95% CI: 37109). The median overall survival couldn’t be evaluated by KaplanMeier method, because the patients were followed until disease progression. After 63 weeks, 80% of patients were alive (95% CI: 60%90%) and after 122 weeks ,75% of patients were alive (95% CI: 55%88%).
ConclusionsSpecifically, no new Avastin safety signals were obser
ved. 88.89% of patients had very good and good tolerability at the end of the therapy. Safety and efficacy results were consistent with phase III data, further confirming the safety and efficacy of Avastin in combination with standard chemotherapy in a broad HER2 negative breast cancer population of patients, representative for routine oncology practice.
www.revista-hipocrate.ro REZUMAT
Noi standarde în prevenirea evenimentelor scheletale asociate tumorilor solide: denosumab
(Xgeva®), la pacien]ii cu metastaze osoasel Dana St`nculeanu MD PhD
Metastazele osoase apar frecvent la pacien]ii cu cancer avansat. Aproape 100% dintre pacien]ii cu mielom multiplu, 6575% dintre cei cu cancer de sân sau prostat` [i 3040% dintre cei cu cancer pulmonar dezvolt` metastaze osoase. Jum`tate dintre ace[ti pacien]i dezvolt` una sau mai multe complica]ii, denumite generic evenimente asociate scheletului skeletal related
events (SRE). Acestea sunt: fractura patologic`, compresia medular`, chirurgia osoas` [i radioterapia paliativ` osoas`. Din anul 2002, inciden]a SRE a fost folosit` ca indice compozit, în studiile desf`[urate pentru a reduce complica]iile scheletice la pacien]ii cu metastaze osoase. SRE determin` morbidit`]i suplimentare, afecteaz` calitatea vie]ii [i reduc supravie]uirea.
Tratamentul cu bisfosfona]i reprezint` o strategie important` în reducerea SRE la pacien]ii cu metastaze

Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România
Reclama

| Septembrie 201214
osoase. Cu toate acestea, bisfosfona]ii reduc inciden]a SRE cu numai 3040% fa]` de placebo, determin` apari]ia reac]iilor adverse la infuzie, a osteonecrozei de maxilar (osteonecrosis of the jaw ONJ) [i necesit` monitorizarea frecvent` a func]iei renale(1).
Receptor activated nuclear factor kappaB ligand (RANKL), unul dintre mediatorii diferen]ierii osteoclastelor, atrage de asemenea [i celulele tumorale la nivel osos care, la rândul lor, activeaz` celulele stromale care produc [i mai mult RANKL, creând un cerc vicios al activ`rii osteoclastice [i distrugerii osoase 1821. Denosumab (Xgeva®) este un anticorp monoclonal complet uman împotriva RANKL, care a demonstrat eficien]` în reducerea markerilor osteolitici [i a inciden]ei SRE. Acesta este administrat subcutanat [i nu este excretat prin rinichi un posibil avantaj pentru pacien]ii cu insuficien]` renal` cronic`(1).
Trei studii controlate au evaluat eficien]a tratamentului cu denosumab (Xgeva®) comparativ cu acidul zoledronic în reducerea inciden]ei SRE la pacien]i cu cancer de sân, prostat`, respectiv alte tumori solide în afar`
de sân [i prostat`, inclusiv mielom. Rezultatele au ar`tat c` denosumab (Xgeva®) este superior acidului zoledronic în prelungirea timpului pân` la apari]ia primului SRE, dar [i în reducerea inciden]ei SRE(2, 3, 4). Analiza combinat` (prespecificat`) a celor trei studii a ar`tat c` denosumab prelunge[te supravie]uirea f`r` eveniment cu 8,2 luni [i reduce riscul de apari]ie a unui SRE cu 17%(5). Nu sau înregistrat diferen]e semnificative legate de inciden]a evenimentelor adverse, inclusiv a ONJ, între denosumab (Xgeva®) [i acidul zoledronic.
În concluzie, inhibarea RANKL cu denosumab (Xgeva®) reprezint` o op]iune nou`, superioar` de tratament pentru prevenirea SRE la pacien]ii cu cancer avansat [i metastaze osoase.
BIBLIOGRAFIEPeddi et al, 2012; Can Treat RevStopeck A et al, 2010; JCOFizazi K et al, 2011; Lancet Henry DH et al, 2010; JCOLipton A et al, 2012;Eur J Can
www.revista-hipocrate.ro REZUMAT
New Approaches in Immunotherapy for Advanced Melanoma
l Dr. Kaan Harmankaya MD
Kaan Harmankaya obtained his MD and completed his doctoral thesis within the field of dermatology, at the Medical University of Vienna, Austria, in 2005. Since 2006, Dr Harmankaya has held an Assistant Medical Doctor position within the Department of Dermatology, and during 2008–2009, he furthered his medical dermatologic training, holding an Internship position in internal medicine within the Department of Internal Medicine I, Division of Oncology, the Medical University of Vienna.
Dr. Harmankaya subsequently obtained his Austrian Board Certification for Dermatology and Venerology in 2011. He is a member of the Austrian Society for Dermatology and Venereology, and the German Cancer Society. Dr. Harmankaya has coauthored several publications and abstracts. He has been both a subinvestigator and study coordinator for more than ten international multicenter clinical trials in stage IIIIV melanoma, and his scientific research interests include dermatooncology, the treatment of metastatic melanoma and the cutaneous side effects of therapies in oncology. Personally he has treated and managed more than 60 patients with distant metastatic melanoma in various clinical settings and protocols, including with antiCTLA4 antibodies.
Ipilimumab is the first immunomodulating agent which significantly improves overall survival in two large randomized controlled phase III trials for patients suffering from distant metastatic melanoma. In studies MDX01020,
which have led to the approval of the compound, patients in a second line treatment setting were randomized into a three arm design, comparing monotherapy with a gp100 vaccine vs. a gp100 vaccine plus Ipilimumab 3mg/kg versus Ipilimumab 3mg/kg alone. A twoyear survival rate of 24%, median overall survival of 10,1 months and a disease control rate of 28,5% for patients in the Ipilimumab alone arm could be achieved.
Ipilimumab monotherapy is a monoclonal antibody directly inhibiting the CTLA4 receptor, expressed on Tcells. It is supposed to lead to increased Tcell activation and proliferation, through which antineoplastic activity against tumor cells is enabled. In the currently approved treatment regimen, Ipilimumab is administered i.v. at 3 mg/kg, in an interval of 21 days for four doses.
Radiologic assessments are to be performed after three months of therapy (at week 12) and, if necessary, at a later time point, to confirm a possible disease progression. Caused by the immunologic mode of action of the drug, antitumor response might be associated with an initial increase in size of tumor metastasis or even growth of new lesions, before leading to tumor shrinkage. These unique clinical characteristics of Ipilimumab therapy have led to the development of immunerelated response criteria, which are a hallmark in the radiological assessment of those patients.
Blocking the CTLA4 receptor and releasing activated Tcells does not only lead to antitumor activity, but also immunologically trigger side effects, called immunere

Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România
Reclama

| Septembrie 201216
l Dr. Adina Croitoru
În lume sunt diagnosticate anual aproximativ un milion de cazuri noi de cancer colorectal, cu circa 500.000 de decese din aceast` cauz`(1). De[i prognosticul bolii metastatice este rezervat, cu o supravie]uire la 5 ani de 58%, descoperirile succesive cu încorporarea agen]ilor terapeutici ]inti]i, în ultimii 20 de ani, au indus o cre[tere a supravie]uirii în cancerul colorectal metastatic de la aproximativ 36 luni la 2428 de luni(2).
Panitumumab (Vectibix®) este un anticorp monoclonal complet umanizat care se leag` specific de receptorul factorului de cre[tere al epidermei (EGFR epidermal growth factor receptor). Dezvoltat de Amgen, a fost aprobat înc` din 2006 de c`tre FDA pentru tratamentul pacien]ilor cu cancer colorectal metastatic (mCRC) care exprim` EGFR [i care au progresat sub regimuri anterioare de chimioterapie, cu demonstrarea unei supravie]uiri f`r` progresia bolii (PFS) de 8 s`pt`mâni(3). Panitumumab a fost primul anticorp monoclonal care a demonstrat utilizarea KRAS ca test predictiv. Ca urmare, FDA a modificat în anul 2009 indica]iile, astfel încât panitumumab se recomand` doar pacien]ilor care nu au muta]ie la nivelul genei KRAS (se folose[te [i termenul WildType KRAS).
Ca [i la bevacizumab, anticorpii antiEGFR par a fi mai eficien]i când sunt utiliza]i în combina]ie cu regimurile de chimioterapie. Dou` mari trialuri clinice randomizate au investigat panitumumab în combina]ie cu FOLFOX în linia Ia, respectiv cu FOLFIRI în linia a IIa de tratament pentru mCRC.
În aceste studii, combina]iile au ar`tat cre[terea supravie]urii f`r` progresia bolii (PFS) vs regimurile simple FOLFOX sau FOLFIRI. A mai fost observat` [i îmbun`t`]irea r`spunsului tumoral prin ad`ugarea de panitumumab (Vectibix®) la FOLFIRI. Ca [i în trialurile cu monoterapie, beneficiile clinice asociate terapiei cu panitumumab (Vectibix®) au fost vizibile doar la pacien]ii cu tumori WTKRAS. Toxicit`]ile observate în timpul tratamentului cu panitumumab (Vectibix®) combinat cu FOLFOX sau FOLFIRI include mai ales toxicitatea cutanat` [i gastrointestinal`(4).
Beneficiile utiliz`rii panitumumab în cancerul colorectal metastatic
www.revista-hipocrate.ro REZUMAT
lated adverse events (irAEs). They might occur in various organ systems, often mimicking commonly known autoimmune disease. Most frequently, they arise in the GItract (diarrhea, colitis), the liver (hepatitis with elevated LFTs), endocrine organs (hypophysitis or thyreoiditis) or
the nervous system (neuropathy, GuillainBarré syndrome or myasthenia gravislike symptoms). Treatment guidelines using systemic corticosteroid administration to counter various irAEs exist and need to be followed meticulously, in order to avoid increased morbidity for the patient.
BIBLIOGRAFIEJemal A, et al. Cancer statistics, CA Cancer J Clin 2010; 60:277-300.Gallagher DJ Metastatic colorectal cancer: from improved survival to potential cure. Oncology 2010; 78:237-48.Van Cutsem E, et al. Open-label phase III trial of panitumumab plus best supportive care compared with best supportive care alone in patients with chemotherapy-refractory metastatic colorectal cancer. J Clin Oncol 2007; 25:1658-64Peeters M et al. Panitumumab in Combination With Cytotoxic Chemotherapy for the Treatment of Metastatic Colorectal Carcinoma. Clinical Colorectal Cancer, 2012; 1 1(1): 14-23
Recent Recommendation for the Treatment of Neuroendocrine Tumorsl Dr. Doina Elena Motan Ganea Spitalul Jude]ean de Urgen]` “Sf. Ioan cel Nou”, Suceava
Neuroendrocrine tumors (NETs) are fairly rare neoplasms. Although recognized for at least one century, they remain orphan tumors, about which little is known. Disappointingly, survival of patients with NETs did not change appreciably over the past three decades, in either the USA or UK.
Many different types of physicians manage NETs, including endocrinologists, gastroenterologists, oncologists,
interventional radiologists and surgeons. Moreover, strategies vary depending on tumor type, spread, general health of the patient and predominant symptoms.
From the therapeutic point of view, surgery is nowadays more extensive, aiming at reducing the tumor mass, in patients who could not be cured by surgery alone. Other means for tumor reduction are liver dearterialization by embolization with starch spheres.
The medical treatment of neuroendocrine tumors has made a real break through with the introduction of somatostatin analogues, particularly octreotide, and in present day, most of the hormonally related symptoms can be con

Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România
Reclama

| Septembrie 201218
trolled by this kind of treatment. Octreotide has also shown to be an inhibitor of tumor growth, becoming the standard treatment for neuroendocrine tumors of gastrointestinal origin. The use of longacting formulation of somatostatin analogues significantly improved quality of life for patients with neuroendocrine tumors.
Chemotherapy, such as streptozotocin plus 5fluorouracil (5FU) or doxorubicin, is used for grade3 Gl NET; is also used as firstline treatment in malignant endocrine pancreatic tumors, but it is combined with concomitant somatostatin analogue treatment. A comparison between treatments is difficult to make, because of heterogeneous patients and few randomised trials.
New targeted treatments as everolimus, an oral inhibi
tor of the mammalian target of rapamycin (mTOR), has shown antitumor activity in patients with advanced pancreatic neuroendocrine tumors. In combination with octreotide, everolimus improved progressionfree survival in patients with advanced neuroendocrine tumors, associated with carcinoid syndrome. According with these recent findings from clinical trials, the international guidelines (NCCN, NANETS and ENETS) were changed.
The development of centers of excellence and NET clinical teams to coordinate multicentre studies, extended clinical and tissue databases and, ultimately, development of molecularly targeted therapeutics are needed to advance the treatment and improve survival for patients with NETs
l Prof. Dr. Manuela Schmidinger,Medical University Vienna, Vienna, Austria
Last 6 years saw tremendous changes of treatment dogma in metastatic renal cell carcinoma. As a result of availability of many therapeutic options, the significance of treatment management, a noteworthy part in itself in oncology, grew ever more important. Maximizing clinical benefit is of paramount importance. However, side
effects may lead to dose reduction and treatment interruption/discontinuation, if not prevented or managed properly.
This presentation describes the scientific rationale that demonstrates the importance of dosing and treatment duration. Treatment management algorithms of the most important adverse events are provided and all is exemplified with a wealth of data from clinical cases. ESMO 2012 latest information are also covered.
Therapy Management in mRCC: State of the Art in 2012
www.revista-hipocrate.ro REZUMAT
l Prof. Dr. Tudor Ciuleanu, Institutul Oncologic “Prof. Dr. Ion Chiricu]̀ ”, Cluj, România,
Sunitinib is an oral, multitargeted receptor tyrosine kinase inhibitor approved for the treatment of advanced and/or metastatic RCC. Sunitinib is recommended in international treatment guidelines as first line therapy for mRCC.
A randomized phase III trial of sunitinib compared
with interferon alfa as first line treatment for metastatic renal cell carcinoma showed superiority of sunitinib over IFN in progressionfree survival time (11 vs. 5 months), by independent, thirdparty radiologic assessment. Final overall survival analyses showed that sunitinib treatment was associated with longer survival compared with IFNalfa (26.4 vs. 21.8 months, respectively). Here we present the results of Cluj Oncology Institute experience in the same setting as the pivotal study.
Sunitinib: proven efficacy in real life practice
l Conf. Dr. Dana St`nculeanu Institutul Oncologic „Prof. Dr. Al. Trestioreanu”, Bucure[ti, România
mTOR inhibitors addresses mRCC with a different mechanism of action than tyrosine kinase inhibitors. Through inhibition of mTOR complexes, they stop various intracellular processes that otherwise would lead to the activation of cell proliferation, angiogene
sis and metastasis.Temsirolimus is the first mTOR inhibitor appro
ved for the treatment of metastatic renal cell carcinoma in poor risk patients. Safety profile of mTOR inhibitors is a distinct one and needs to be approached carefully, in order to maximize clinical benefit. The efficacy and safety results from a pivotal phase III study are presented, along with personal clinical experience.
Temsirolimus, Effective Therapy Management using a Powerful mTOR Inhibitor Case Study

Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România
Reclama

| Septembrie 201220
l Michael Untch MD PhD
HannaH StudySubcutaneous versus intravenous administration of
(neo) adjuvant trastuzumab in patients with HER2positive, clinical stage I–III breast cancer (HannaH study) is a phase 3, openlabel, multicenter, randomized trial. The IV formulation of Herceptin is the standard of care for HER2positive BC. Herceptin IV is administered over 90 minutes (initial dose) or 30 minutes (maintenance dose). Dosage is based on body weight. The Herceptin SC formulation, which has been developed as an alternative to the IV formulation, is administered in less than 5 minutes, thus offering the potential for improved convenience, compliance and reduced medical resource utilisation.
The Herceptin SC formulation requires no loading dose and is administered as a fixed dose (600 mg). Herceptin SC formulation contains recombinant human hyaluronidase (rHuPH20), which facilitates the absorption of Herceptin into the circulation and allows the 5 mL injection volume to be administered comfortably via the SC route. The purpose of the study was to demonstrate the noninferiority of Herceptin SC fixeddose formulation, compared with the standard Herceptin IV formulation, based on the coprimary endpoints:
Serum Ctrough of Herceptin predose at Cycle 8 (before surgery;
pCR, defined as the absence of invasive neoplastic cells in the breast.
Secondary endpoints reported in this paper include total pCR (absence of invasive neoplastic cells in the breast and ipsilateral lymph nodes) and safety (including immunogenicity).
Patients with HER2positive, operable, locally advanced or inflammatory BC received 8 cycles of neoadjuvant chemotherapy, consisting of 4 cycles of docetaxel (75 mg/m2) followed by4 cycles of FEC (500/75/500 mg/m2).
Patients were randomized (1:1) to receive 8 cycles of Herceptin (q3w) administered as either:
Herceptin IV formulation (8 mg/kg initial dose, followed by 6 mg/kg maintenance dose);
Herceptin SC fixeddose formulation (600 mg) administered into the patient’s thigh using a manual, handheld syringe. Herceptin was administered concurrently with chemotherapy.
After surgery, patients continued to receive Herceptin, as per the initial randomization, to complete one year of treatment.
The primary analysis was conducted when all patients had completed surgery and at least 100 patients in each arm had completed one year of treatment.
596 patients were enrolled at 81 centres in Europe (47), Asia (12) South and Central America (17), North
America (1) and Africa (4). Surgery data were available for 278 patients (93%) in the Herceptin IV arm and 275 patients in the Herceptin SC arm (93%). Baseline demographics and tumor characteristics were similar between treatment arms. At the time of the analysis, 116 patients from each arm had completed adjuvant Herceptin therapy.
Cleopatra StudyThis analysis of overall survival in the CLEOPATRA
study crossed the prespecified boundary showing that the combination of Perjeta, Herceptin and docetaxel chemotherapy significantly improved overall survival in people with HER2positive mBC, compared with Herceptin and chemotherapy. Overall survival is a secondary endpoint of the CLEOPATRA study.
The final progression free survival (PFS, the primary endpoint) and safety profile data from the CLEOPATRA study were published in December 2011 in the New England Journal of Medicine and demonstrated that people who received Perjeta in combination with Herceptin and docetaxel chemotherapy had a statistically significant 38 percent reduction in the risk of their disease worsening or death (progressionfree survival; PFS, HR=0.62, pvalue<0.0001) compared to people who received Herceptin and chemotherapy plus placebo. The median PFS improved by 6.1 months, from 12.4 months for people who received Herceptin and chemotherapy plus placebo, to 18.5 months for those who received Perjeta, Herceptin and chemotherapy.
In CLEOPATRA, the most common adverse reactions (rate greater than 30 percent) seen with Perjeta in combination with Herceptin and docetaxel chemotherapy were diarrhea, hair loss, low white blood cell count with or without fever, upset stomach, fatigue, rash and peripheral neuropathy (numbness, tingling or damage to the nerves). The most common Grade 3–4 adverse reactions (rate greater than 2 percent) were low white blood cell count with or without fever, decrease in a certain type of white blood cell, diarrhea, damage to the nerves, decrease in red blood cell count, weakness and fatigue.
CLEOPATRA (CLinical Evaluation Of Pertuzumab And TRAstuzumab) is an international, Phase III, randomized, doubleblind, placebocontrolled study. The study evaluated the efficacy and safety profile of Perjeta combined with Herceptin and docetaxel chemotherapy compared to Herceptin and chemotherapy plus placebo in 808 people with previously untreated HER2positive mBC or with HER2positive mBC that had recurred after prior therapy in the adjuvant or neoadjuvant setting.
The primary endpoint of the study was PFS, as assessed by an independent review committee. Secondary endpoints were overall survival, PFS by investigator assessment, safety profile, overall response rate (ORR), duration of the response and time to symptom progression.
Temsirolimus, Effective Therapy Management using a Powerful mTOR Inhibitor - Case Study
www.revista-hipocrate.ro REZUMAT

Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România
Reclama

| Septembrie 201222
l Dr. Sophie Leymann, Senior Regional Medical Affairs Director, Oncology, EURIT region, Pfizer, Belgium
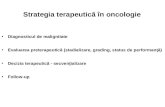
Personalized medicine is one of the greatest promises of the future. Tailoring medical treatment to the individual characteristics of each patient will improve drastically clinical outcome. Lung cancer is one area in which many advances were taken in the last few years. Driver mutations associated with lung cancer
were discovered and targeted drugs directed to the resulting oncoprotein were developed. Improved outcomes were, thus, achievable for the patients with those specific mutations. One can infer from this the importance of identification of these mutations in lung cancer patients.
Presentation outlines the definition of Personalized Medicine, the evolution towards biomarker driven therapy and what are the challenges and opportunities of personalized medicine in cancer.
The Emerging Role of Personalized Medicine in Cancer
www.revista-hipocrate.ro REZUMAT
l Dr. Patrick Pauwels,Antwerp University Hospital, Antwerp, Belgium
Molecular testing in NSCLC is of paramount importance if targeted agents are to be used. As only the group that has a specific oncogenic driver mutation will respond to the specifically designed therapeutic agent, correct identification is mandatory. EGFR and ALK mutati
ons are known to be key drivers of the lung oncogenesis. Due to differences and difficulties in various types of molecular testing, extensive expertise is required from all involved counterparts.
This presentation sketches out technical aspects of molecular testing, recommendations for mutation testing and a testing algorithm in nonsmall cell lung cancer.
Molecular Testing in NSCLC
The Efficacy and Cost of Biological Targeted Agents in Oncology
l Doru Paul, MD HematologyOncology Attending NSLIJ Monter Cancer Center
Significant advances in molecular biology over the past fifteen years led to the development of rationally designed new classes of drugs that target specific key factors involved in the malignant process. The term “biological targeted therapy” refers to this new generation of cancer drugs designed to interfere with a specific molecular target (typically a protein) that has been proved to have a critical role in tumor growth or progression(1).
The introduction of biological targeted agents has revolutionized the management of certain cancer types and has contributed to recent improvements in survival rates of cancer patients, in certain subgroups of “novel nosological entities”(80). It is important to note that although the molecular target of these agents is known and, in general, these agents act more selectively on the tumor cells than che
motherapy, they may still have significant sideeffects.In a recent longterm followup data on the imatinib
treatment of patients with chronic myelogenous leukemia (CML), the overall survival of patients was very impressive, 8090% of the patients taking this drug being alive at 10 years(11). The fact that the prognostic of patients with CML has improved significantly after the introduction of imatinib on the market should not make us extrapolate positive results of this level of magnitude to other tumor types. Imatinib success seems to be rather the exception than the rule(12). The reason for imatinib efficacy in CML is probably related to the special pathophysiology of this disease; in CML, the tumors become “addicted” to a unique, constitutively active ABL kinase that has a direct, causal relationship with the development of CML(13) Mice made transgenic with BCR/ABL DNA construct develop leukemia shortly after birth(77). In contrast to this idiosyncratic pathologic mechanism, solid tumors are much more complex than CML, each solid tumor is unique and bears a much hi

Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România
Reclama

| Septembrie 201224
gher number of mutations than CML. For example, on average, breast tumors may have at least 105 mutated genes and colorectal cancer may have at least 81 mutated genes from which an average of 20 and 14, respectively, are cancer genes directly involved in the malignant process(14). Individual pancreatic cancers may have at least 63 mutations and glioblastoma multiforme tumors may bear at least 47 mutations(15). This complexity and heterogeneity makes solid tumors much more difficult to treat than CML.
It became quickly clear that the benefit of these “smart agents” that target epidermal or vascular growth factors and tyrosine kinases is restricted to only a subgroup of patients, and the quality of life of some patients may be even worsened by taking them. For example, it has been estimated that in US approximately 100,000 patients with metastatic colorectal cancer with tumors harboring mutant KRAS have received unhelpful and potentially detrimental therapy before clinical studies had shown that these patients do not benefit from cetuximab and, in fact, they may have been harmed by taking it(12).
Also, the added value of biological targets to the armamentarium of contemporary cancer treatment comes with a monetary price which is not at all negligible. All these products are expensive and, unfortunately, their market cost does not match their clinical benefit, that in some cases is modest, at best. Of course, as human beings we believe that every life, is unquestionably, “of infinite value and we naturally avoid confronting the tension between not wanting to put a value on a life and having limited resources”(81). It should be made clear that we do not advocate with holding potentially life prolonging medications from patients that may benefit from them. On the other hand, in order to better plan the best available care for the highest number of cancer patients and better allocate the resources that may be scarce and much lower than the needs, we should also be knowledgeable of the financial aspects of these agents. More than 90% of the biological target agents approved by the FDA in the last decade cost more than $20,000 for a 4month course of treatment(4). These approvals and the use of these drugs by oncologists in US implicitly signals to pharmaceutical companies our tolerance for high pricing, and “they set a higher threshold for what society considers acceptable”(81). According to the United States Census Bureau, the median yearly household income in US is approximately 52,000(78) which disturbingly contrasts the cost of the majority of biological agents is significantly higher than this figure. For example, the cost of four months treatment of ipilimumab used in metastatic melanoma is ~$100,000 and three doses of sipoluecel T used in metastatic prostate cancer cost ~$93,000.
Given all these complex medical, social and economical issues, we performed a systematic review of the FDA approved biological agents in US(3) and investigated both their potential benefits, measured by the most significant endpoints reported in the clinical trials i.e., overall survival (OS) and progression free survival (PFS) and their current market cost(4).
At present, in August 2012, in US there are twenty FDA approved biological agents for the treatment of solid tu
mors. Here is a brief overview of the evidence of the benefit of these 20 drugs in different cancer types, as supported by the currently published Phase III studies. For comparison, their US market price is included.
1. Trastuzumab (Herceptin)Trastuzumab is FDA approved for metastatic breast
cancer since September 1998 and since November 2006 for the adjuvant treatment of HER2positive breast cancer. It is also approved since October 2010 to treat HER2positive gastroesophageal junction and gastric adenocarcinoma.
In a pivotal phase III trial, trastuzumab administered in firstline in combination with chemotherapy to the patients with HER2positive metastatic breast cancer significantly prolonged time to disease progression (TTP) (7.4 versus 4.6 months) and OS (25 versus 20 months), when compared to chemotherapy alone(19).
For the use of Herceptin in the adjuvant setting, the investigators from the National Surgical and Bowel Project (NSABP) and the North Central Cancer Treatment Group (NCCTG) reported a combined analysis of the control arms for 2 trials (NSABPB31, 1736 patients plus N 9831, 1615 women, respectively) versus the concurrent trastuzumab groups from each trial. The Pooled analysis showed that adjuvant trastuzumab combined with paclitaxel chemotherapy resulted in a greater than 50% reduction in recurrence risk: fouryear PFS 86% versus 73%, hazard ratio (HR) of 0.51) and a 37% reduction in risk of death (fouryear OS 93% versus 89%, HR 0.63)(20). A metaanalysis that included 8 adjuvant studies and approximately 12,000 patients also significantly favored the trastuzumabcontaining regimen both for OS and PFS(21).
Trastuzumab is also approved for the treatment of metastatic gastric cancer. In the TOGA trial, that randomized 594 patients, median OS was 13.8 months (95% CI 1216) in the trastuzumab plus chemotherapy arm, compared with 11.1 months (1013) in the chemotherapy alone arm (HR 0.74; 95% confidence interval (CI) of 0.600.91; p=0.0046)(22).
Cost. 440 mg of Herceptin solution costs $3675.85. The current adjuvant treatment recommendation is an initial loading dose of 4 mg/kg followed by 2mg/kg weekly for 12 weeks followed by 6mg/kg up to 52 weeks (one year). The total cost for the adjuvant treatment using the currently recommended adjuvant treatment protocol is $69,841.15.
2. Imatinib mesylate (Gleevec)Imatinib received FDA orphan drug approval for all
stages of CML since May 2001. It is also approved since February 2002 to treat gastrointestinal stromal tumor (GIST). Since October 2006, it is also approved to treat unresectable dermatofibrosarcoma protuberans (DFSM).
For metastatic GIST, historical data shows a median OS of 19 months for all patients with metastatic disease and 9 months for patients with metastatic disease and local recurrence(17). In a Phase 3 study that enrolled 746 patients with advanced unresected GIST, the median PFS was 18 months for patients on the standarddose arm, and
www.revista-hipocrate.ro REZUMAT

Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România
Reclama

| Septembrie 201226
20 months for those receiving highdose imatinib. Median OS was 55 and 51 months, respectively(18). Thus, in the absence of controlled studies, historical comparison suggests that firstline treatment with imatinib may improve survival by approximately threefold compared with standard of care in the preimatinib era. In the adjuvant setting, for resected GIST tumors, imatinib significantly prolonged relapsed free survival (RFS) compared with placebo (98% vs. 83% at 1 year; overall hazard ratio 0.35; onesided p<0.0001). Overall survival (OS) was though similar (99.2% vs. 99.7% at 1 year; HR 0.66; p=0.47)(16). On the other hand, it has been shown that the 36 months of Gleevec treatment significantly prolonged OS compared to 12 months of Gleevec treatment with a HR of 0.45 (95% CI: 0.22, 0.89), p=0.0187 (Package insert data). For DFSM there is data only in 18 patients. Twelve of these 18 patients either achieved a complete response (7 patients) or were made disease free by surgery after a partial response (5 patients, including one child) for a total complete response rate of 67%. A further 3 patients achieved a partial response, for an overall response rate of 83%. Of the 8 patients with metastatic disease, five responded (62%), three of them completely (37%) (Package insert data).
Cost. 30 tablets of 100 mg cost $1640.92; 30 tablets of 400 mg cost $5,963.04. The minimum cost of a month of treatment is $5,963.04. The recommended dose for treatment of GIST is 400 mg/day. This dose may be escalated to 800 mg/day.
3. Cetuximab (Erbitux)Cetuximab was FDA approved in colorectal cancer in
February 2004 in combination with irinotecan for patients with metastatic colorectal carcinoma who have been refractory to irinotecan based chemotherapy alone. In July 2009, there were some changes in the label as following: cetuximab, as a single agent, was indicated for the treatment of metastatic colorectal cancer after failure of both irinotecan and oxaliplatinbased regimens. Cetuximab, as a single agent, was also indicated in the treatment of metastatic colorectal cancer in patients who are intolerant to irinotecanbased regimens. Also a note was added to the label in July 2009 stating that retrospective subset analyses of metastatic or advanced colorectal cancer trials have not shown a treatment benefit for cetuximab or panitumumab in patients whose tumors had KRAS mutations in codon 12 or 13 and the use of cetuximab and panitumumab are not recommended for the treatment of colorectal cancer with these mutations.
In 2004, a Phase III randomized study established the role of cetuximab in combination with irinotecan in irinotecan refractory patients with metastatic colorectal cancer. 329 patients whose disease had progressed during or within three months after treatment with an irinotecanbased regimen were randomized to receive either cetuximab and irinotecan or cetuximab monotherapy. The median time to progression was significantly greater in the combinationtherapy group (4.1 vs. 1.5 months, P<0.001 by the logrank test), but median OS was not statistically significant (8.6 months in the combinationtherapy group and 6.9 months
in the monotherapy group (P=0.48). Despite of the lack of benefit in OS, cetuximab received FDA approval(76). More recently, the benefit of cetuximab in metastatic colorectal cancer has been addressed in two trials: the CRYSTAL(66, 67) and OPUS(68). In the CRYSTAL study for patients with wildtype KRAS, the benefit of cetuximab included a significantly better OS (median 23.5 versus 20 months), PFS (9.9 versus 8.4 months), and better response rate(66,67). In this study, 1198 patients were randomized and 676 patients had wild typeKRAS (316 in the cetuximab + chemo arm and 350 in the chemo alone arm). On the other hand, in the OPUS study there was no significant difference in PFS between the two treatment arms. When retrospective efficacy analyses were carried out in the KRAS population of the OPUS study according to KRAS mutation status, an increase in the PFS was detected in the cetuximab + FOLFOX arm (8.6 months vs 5.5 months. HR:1.83, p=0.02)(69). Two other large randomized studies failed to detect any improvement in the OS or PFS adding cetuximab to oxaliplatin based chemotherapy in frontline metastatic colorectal cancer. The COIN study accrued 1,630 patients and 729 had wild typeKRAS tumors(70). The Nordic VII trial enrolled 566 patients and 40% of them (303) had wild typeKRAS tumors(71). No benefit from adding cetuximab was found in any of these studies. Based on this data, it may be argued that cetuximab benefit is seen mostly when used in combination with irinotecan based chemotherapy.
In squamous cell cancer of the head and neck (SCCHN), cetuximab is approved since March 2006, in combination with radiotherapy, for the treatment of locally or regionally advanced disease. It is also approved since November 2011 in recurrent locoregional disease or metastatic disease, in combination with platinumbased therapy with 5FU and also as single agent in recurrent or metastatic squamous cell carcinoma of the head and neck progressing after platinumbased therapy.
Cetuximab was evaluated in a multinational trial, in combination with radiotherapy, in locoregionally advanced cancers of the oropharynx, hypopharynx, or larynx. With a median followup of 54 months, the median duration of OS was 49 months among patients treated with combined therapy and 29.3 months among those treated with radiotherapy alone (HR for death, 0.74; P=0.03). Locoregional control rates were also significantly better. The median duration of locoregional control was 24.4 months among patients treated with cetuximab plus radiotherapy and 14.9 months among those given radiotherapy alone (HR for locoregional progression or death, 0.68; P=0.005)(74). An underpowered subset analysis showed that patients with oropharyngeal tumours, early AJCC T, stage (T1–3), treatment in the USA, concomitant boost, advanced AJCC N stage (N1–N3), high KPS (90–100), male sex, and age less than 65 years were factors associated with a potential increased benefit from cetuximab combined with radiotherapy versus radiotherapy alone. However, the trial was not powered for this unplanned subgroup analysis and, therefore, these observations should be interpreted with caution(75).
In a phase III trial, 442 patients with recurrent or me
www.revista-hipocrate.ro REZUMAT

Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România
Reclama

| Septembrie 201228
tastatic head and neck cancer were assigned to a firstline regimen of platinum (cisplatin or carboplatin plus fluorouracil every three weeks) with or without cetuximab. Adding cetuximab to platinumbased chemotherapy with fluorouracil significantly prolonged the median OS from 7.4 months in the chemotherapyalone group to 10.1 months in the group that received chemotherapy plus cetuximab (HR for death, 0.80; 95% confidence interval, 0.64 to 0.99; P=0.04). The addition of cetuximab prolonged the median PFS time from 3.3 to 5.6 months (HR for progression, 0.54; P<0.001) and increased the response rate from 20% to 36% (P<0.001)(72).
Cetuximab administered as a single agent was studied in a multicenter Phase II clinical trial in 103 patients with recurrent or metastatic SCCHN. All patients had documented disease progression within 30 days of a platinumbased chemotherapy regimen. Patients received a 20mg test dose of cetuximab on Day 1, followed by a 400 mg/m2 initial dose, and 250 mg/m2 weekly until disease progression or unacceptable toxicity. The median age was 57 years, 82% were male, 100% caucasian, and 62% had a Karnofsky performance status of more than 80. The objective response rate was 13% (95% confidence interval 7%–21%). Median duration of response was 5.8 months (range 1.2–5.8 months). In the singleagent phase, response rate was 13%, disease control rate (complete response/partial response/stable disease) was 46%, and median time to progression (TTP) was 70 days. Median OS was 178 days(73).
Cost. 100 mg/50 ml cost $575.99; 200 mg/100 ml cost $1061.94. The average cost for a month treatment is approximately $10,000. The initial loading dose is 400 mg/m2 followed by a weekly 250 mg/m2.
4. Panitumumab (Vectibix) Panitumumab is FDA approved since September 2006
in US as a single drug, as a last option to treat some patients with KRAS nonmutated metastatic colon cancer with disease progression on or following fluoropyrimidine, oxaliplatin, and irinotecancontaining chemotherapy regimens. The effectiveness of panitumumab for the treatment metastatic colorectal carcinoma is based on PFS data only. Currently no data is available that demonstrate an improvement in diseaserelated symptoms or increased survival with panitumumab. The benefit of panitumumab monotherapy was initially shown in a multicenter trial in which 463 patients refractory to 5FU, irinotecan, and oxaliplatin were randomly assigned to best supportive care (BSC) with or without panitumumab (6 mg/kg every two weeks). The objective response rate with panitumumab was 10%, and 27% had stable disease; the corresponding rates with BSC alone were 0 and, respectively, 10%. Patients receiving panitumumab were significantly more likely to be alive and progressionfree at eight weeks (49 versus 30 %). Median PFS time was 8 weeks (95% CI, 7.9 to 8.4) for panitumumab and 7.3 weeks (95% CI, 7.1 to 7.7) for BSC. Mean (standard error) PFS time was 13.8 (0.8) weeks for panitumumab and 8.5 (0.5) weeks for BSC. No difference was observed in OS (HR, 1.00; 95% CI, 0.82 to 1.22), which may have been confounded by 76% patients from the BSC group crossing over to the panitumumab arm(45).
Cost. 100 mg/5ml cost $951.99, 400 mg/20 ml cost $4349.40. The average cost for a month treatment is approximately $10,600. The recommended dose of panitumumab is 6 mg/kg every 2 weeks.
5. Temsirolimus (Torisel)Temsirolimus was FDA approved in May 2007 to
treat patients with advanced renal cell carcinoma (RCC). Temsirolimus was evaluated in a phase III trial in previously untreated poorprognosis patients with metastatic or recurrent RCC were randomly assigned to temsirolimus (25 mg IV/week), temsirolimus (15 mg IV/week) plus IFNa (escalated up to 6 million units three times per week as tolerated), or IFNa monotherapy (escalated up to 18 million units three times per week as tolerated). Temsirolimus as a single agent significantly prolonged the median OS compared to IFNa as a single agent (10.9 versus 7.3 months; HR for mortality 0.73, 95% CI 0.580.92). Also the median PFS of the patients receiving single agent temsirolimus was improved compared to the patients receiving single agent IFNa, according to both investigator and independent radiologic assessment (3.8 versus 1.9 months and 5.5 versus 3.1 months, respectively)(37).
Cost. 1 dose of 25 mg costs $1343.96. The average cost for a month treatment is approximately $5,376. The recommended dose of Torisel is 25 mg once a week.
6. Everolimus (Afinitor)Everolimus was FDA approved in March 2009, to treat
patients with advanced RCC whose disease has progressed after treatment with other therapies and patients with pancreatic neuroendocrine tumors that cannot be removed by surgery, are locally advanced, or have metastasized. In November 2010, it has been approved for patients with subependymal giant cell astrocytoma who also have tuberous sclerosis and are unable to have surgery. It has been also approved in July 2012, for the treatment of postmenopausal women with advanced hormone receptorpositive, HER2negative breast cancer (advanced HR+ BC) in combination with exemestane, after failure of treatment with letrozole or anastrozole.
A randomized Phase III trial compared everolimus with placebo in patients with metastatic renal cell cancer that progressed on vascular endothelial growth factor tyrosine kinase inhibitors (VEGF TKI), (sorafenib, sunitinib) or within 6 months after completing such a therapy. There was no statistically significant difference in OS (median 14.8 versus 14.4 months, HR 0.87), but patients who had been assigned to placebo were eligible for crossover to everolimus when progressive disease developed and 80% of placebo patients received everolimus. The median PFS was 4.9 months (everolimus) versus 1.9 months (placebo) (HR, 0.33; P<0.001) by independent central review and 5.5 months (everolimus) versus 1.9 months (Placebo) (HR, 0.32; P<0.001) by investigators. Also stable disease was more common in the patients receiving everolimus vs the patients receiving placebo (63 and 32%, respectively) (9, 38).
The Radiant3 Study Group evaluated patients with lowgrade or intermediategrade pancreatic neuroendo
www.revista-hipocrate.ro REZUMAT

Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România
Reclama

| Septembrie 201230
crine tumors with radiologic progression within the previous 12 months to receive everolimus, at a dose of 10 mg once daily (207 patients), or placebo (203 patients), both in conjunction with best supportive care. The median PFS was 11.0 months with everolimus as compared with 4.6 months with placebo (HR for disease progression or death from any cause with everolimus, 0.35; 95% CI, 0.27 to 0.45; P<0.001), representing a 65% reduction in the estimated risk of progression or death(39).
Everolimus is also approved in patients with subependymal giant cell astrocytoma (SEGA) who also have tuberous sclerosis (TS) and are unable to have surgery based on the results of a Phase II study. Twentyeight patients were enrolled in the study and ranged in age from 3 to 34 years old. All had a diagnosis of TS and documentation of serial growth (on two successive MRI scans) of a SEGA. The primary end point was the change in volume of the SEGA during 6 months’ treatment, while seizure frequency, neurocognition and quality of life were secondary end points. At 6 months into the study, nine patients (32%) had a greater than 50% reduction in tumor volume of their largest SEGA tumor lesion. Seven of these patients retained the >50% reduction in tumor volume at time of last followup. Patients participating in the study did not develop any new tumors. However, no tumor resolved completely. Based on the encouraging results observed on this study, FDA granted accelerated approval of everolimus for patients with SEGAs that are not candidates for surgical resection(40).
Everolimus has been also approved in July 2012 for the treatment of postmenopausal women with advanced hormone receptorpositive, HER2negative breast cancer (advanced HR+ BC) in combination with exemestane, after failure of treatment with letrozole or anastrozole. In an updated report of the Bolero2 study, PFS by investigator assessment showed a hazard ratio (HR) of 0.44 (95% CI: 0.36–0.53) and a median duration of 7.4 (everolimus+exemestane) vs 3.2 months (exemestane alone) (P<1 x 10–16) and 12month estimate of 31% vs 10%. PFS by central assessment showed an HR of 0.36 (95% CI: 0.28–0.45) and a median duration of 11.0 (everolimus+exemestane) vs 4.1 months (exemestane alone) (P<1 x 10–16)(36).
Cost. 2.5 mg tabs/28 cost $7054.34. 5 mg tabs/28 cost $7187.62, 10 mg tabs/28 cost 7580.37. The average cost for a month treatment is approximately $8,000. The recommended dose is 10 mg once a day.
7. Vandetanib (Caprelsa)Vandetanib was FDA approved in April 2011 to treat
patients with metastatic medullary thyroid cancer who are ineligible for surgery. Vandetanib’s safety and effectiveness were established in a single, Phase III, randomized international study of 331 patients with latestage medullary thyroid cancer. Patients in the study were selected to receive vandetanib or placebo. In this study, there was a significant prolongation of PFS in patients who received vandetanib compared with placebo, with an HR of 0.46 and an estimated 11month prolongation of median PFS. The median PFS was 19.3 months in the placebo group and, although
the median had not yet been reached for the vandetanib group, fitting a statistical Weibull model indicated a predicted median of 30.5 months. OS data were immature at data cutoff and the authors stated that a final survival analysis will take place when 50% of the patients have died(41).
Cost. The price per tablet is $195.00, equating to a cost of $5850 per month. The recommended dose of Caprelsa® is 300mg taken once daily.
8. Vemurafenib (Zelboraf)Vemurafenib was FDA approved in August 2011 to
treat certain patients with inoperable or metastatic melanoma. This smallmolecule drug blocks the activity of a permanently activated mutant form of the serine/threonine kinase BRAF (known as BRAF V600E). A landmark phase III trial compared vemurafenib with dacarbazine in previously untreated patients whose tumors contained the V600E mutation in BRAF. In the BRIM3 trial, 675 patients were randomly assigned to either vemurafenib (960 mg twice a day) or dacarbazine (1000 mg/m2 intravenously every three weeks). Treatment was to be continued until disease progression. All patients had either metastatic disease or unresectable stage IIIC disease (95 and 5 percent, respectively). OS was significantly increased in patients assigned to vemurafenib compared with dacarbazine. The estimated survival rates at 6 months were 84% for patients receiving vemurafenib versus 64% of the patients receiving dacarbazine (HR for death 0.37, 95% CI 0.260.55). PFS was also significantly longer in those initially treated with vemurafenib (median 5.3 versus 1.6 months, HR 0.26, 95% CI 0.200.33). Finally, the objective response rate was significantly higher with vemurafenib (48 versus 4% with a P<0.001)(42).
Cost per month of 480 tabs (120 mg tabs) is $10,748.44. The recommended dose is 960 mg twice a day.
9. Crizotinib (Xalkori)Crizotinib was FDA approved in August 2011 to treat
certain patients with locally advanced or metastatic nonsmall cell lung cancer (NSCLC). This approval is independent on whether or not the patients have received previous treatment for NSCLC. There is no data available demonstrating improvement in patient reported outcomes or survival with criozotinib. The FDA approval is based on response rate rather than survival data(43). This smallmolecule drug inhibits the tyrosine kinase activity of a fusion protein called echinoderm microtubuleassociated proteinlike 4anaplastic lymphoma kinase (EML4ALK), resulting in decreased tumor cell growth, migration, and invasiveness. Crizotinib is recommended for patients with EML4ALK gene rearrangements that are present in approximately 1% of patients with adenocarcinoma of the lung. Crizotinib is a kinase inhibitor indicated for the treatment of patients with locally advanced or metastatic NSCLC that is ALKpositive, as detected by an FDAapproved test. The efficacy of crizotinib was established in two multicenter, single arm studies. In total, these studies included 255 patients, all of whose tumors contained an ALK gene rearrangement, as shown by FISH. Overall, 95% of patients had metastatic disease and 5% had locally advanced NSCLC. The combined objective (complete plus partial) response
www.revista-hipocrate.ro REZUMAT

Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România
Reclama

| Septembrie 201232
rate was 55 percent, the majority of which was achieved during the first eight weeks of treatment. The median durations of response at the time of analysis on the two studies were 42 and 48 weeks, respectively. The majority of these patients were heavily pretreated: 76% had received two or more treatment regimens(43). Retrospective analysis of the results from a nonrandomized, Phase I study suggests improvement in the survival of patients receiving crizotinib. The one and twoyear survival rates for patients treated with crizotinib were 74 and 54%, respectively, with a median follow up of 18 months. For comparison, in a cohort of 36 patients with the ALK fusion oncogene who were not treated with crizotinib, the survival rates at one and two year were 44 and 12%, respectively(44).
Cost of 30 200 mg capsules is $5151.25. The cost of a treatment/month is $10,302.5. The recommended dose is 200 mg po bid.
10. Pertuzumab (Perjeta)Pertuzumab is FDA approved since June 2012, in com
bination with trastuzumab and docetaxel to treat metastatic breast cancer that expresses HER2 and has not been treated with chemotherapy or a HER2directed therapy. Pertuzumab is a monoclonal antibody that binds to HER2 at a region distinct from trastuzumab. This region allows HER2 to interact with other receptors, such as the epidermal growth factor receptor (EGFR), to send growthpromoting signals. In a pivotal Phase III trial, 808 patients with HER2positive metastatic breast cancer were randomized to receive as firstline treatment placebo plus trastuzumab plus docetaxel (control group) or pertuzumab plus trastuzumab plus docetaxel (pertuzumab group). The treatment was given until the time of disease progression or the development of unmanageable toxic effects. The median PFS was 12.4 months in the control group, as compared with 18.5 months in the pertuzumab group (HR for progression or death, 0.62; 95% CI, 0.51 to 0.75; P<0.001). The interim analysis of OS showed a strong trend in favor of pertuzumab plus trastuzumab plus docetaxel(50).
Cost. 30 mg/ml X 14 mls costs $4279.44. The average cost of a treatment/month is $5,700. Initial loading dose is 840 mg followed by 420 mg Q 3 weeks.
11. Lapatinib (Tykerb)Lapatinib is FDA approved since March 2007 for the
treatment of certain types of advanced or metastatic breast cancer. In a randomized Phase III study Tykerb + capecitabine vs capecitabine alone improved time to progression in the combination arm to 8.4 months vs 4.4 months in the capacitabine alone arm. HR 0.49 (95% confidence interval, 0.34 to 0.71; P<0.001). The median OS was 75.0 weeks for the combination arm and 64.7 weeks for the monotherapy arm (HR, 0.87; 95% confidence interval [CI], 0.711.08; p =0.210) (not statistically significant). However, if the 36 patients who crossed over to combination therapy are excluded from the analysis, the combination of lapatinib and capecitabine resulted in a statistically significant improvement in median OS. (75.0 versus 56.4 weeks)(29,30).
Cost of 150 tabs of 250 mg is $3300. The average cost of a treatment/month is $33004000 depending on the combi
nation used. The daily approved dose of lapatinib is 1250 mg (in combination with capecitabine) and 1500 mg (in combination with letrozole).
12. Gefitinib (Iressa)Gefitinib is FDA approved since May 2003 (in areas of
the world where gefitinib is available, it may be used in place of erlotinib) to treat patients with advanced nonsmall cell lung cancer. Gefitinib was originally approved in 2003, but in June 2005, the FDA approved new labeling that limited the approval, i.e., only for patients who are currently benefiting (or have previously benefited) from this agent. The reason for this change is that the post approval phase III placebocontrolled study of gefitinib, the Iressa Survival Evaluation in Lung Cancer (ISEL) trial, was negative showing only a small difference in OS between the experimental arm and placebo (5.6 vs 5.1 months, P = .087)(2). In a pivotal phase III trial study, IPASS, 1217 patients light smokers or no smokers with adenocarcinoma randomized to receive gefitinib or carbotaxol. The study was initially published in New England Journal of Medicine (NEJM) in September 2009, then a followup was published in the Journal of Clinical Oncology in July 2011. Results for PFS: in the subgroup of 261 patients who were positive for the epidermal growth factor receptor gene (EGFR) mutation, PFS was significantly longer among those who received gefitinib than among those who received carboplatinpaclitaxel. In the subgroup of patients with Epidermal Growth Factor Receptor (EGFR) mutation–positive tumors, (HR, 0.48; 95% CI, 0.36 to 0.64; P<0.001; median PFS, 9.5 v 6.3 months) whereas in the subgroup of 176 patients who were negative for the mutation, PFS survival was significantly longer among those who received carboplatinpaclitaxel chemotherapy (HR, 2.85; 95% CI, 2.05 to 3.98; P<0.001; median PFS, 5.5 v 1.5 months). There was no significant difference in OS for gefitinib versus carboplatin/paclitaxel in any subgroup(24). Please note that gefitinib is endorsed by NCCN for use in NSCLC patients with EGFR mutations, but it is not approved by FDA for this indication.
Cost/month of 250 mg (30 tabs) is $1805.91. The approved daily dose of gefitinib is 250 mg po.
13. Erlotinib (Tarceva)Erlotinib is FDA approved since November 2005 to
treat pancreatic cancer that cannot be removed by surgery or has metastasized. A phase III trial from the National Cancer Institute of Canada (NCIC) compared gemcitabine with and without erlotinib and found a benefit in OS in the combination arm of 2 weeks (HR 0.81, p = 0.038, median 6.2 versus 5.9 months, oneyear survival 23 versus 17 percent, respectively). The PFS was also better by 2 weeks in the combination arm(28). Please note that, in lung cancer, erlotinib has three current National Comprehensive Cancer Network (NCCN) indications but only the first two are FDA approved:
1. Erlotinib is approved since April 2010 for maintenance treatment in locally advanced or metastatic nonsmall cell lung cancer. In the SATURN study, 884 patients were analyzable for PFS at ~11.5 months of followup. PFS was significantly longer in patients with EGFRpositive immu
www.revista-hipocrate.ro REZUMAT

Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România
Reclama

| Septembrie 201234
nohistochemistry irrespective of mutational status (median PFS 12.3 vs 11.1 weeks; HR 0·71, 95% CI 0·62–0·82; p<0·0001). OS was also significantly prolonged with erlotinib versus placebo in the intentiontotreat population (median 12 vs 11 months; HR 0.81, 95% CI 0.70–0.75; p=0.0088)(25).
2. Erlotinib is also approved for second and third line treatment in all types of NSCLC, since November 2004. In a study published in the NEJM, PFS for erlotinib versus placebo used in second or third line was 2.2 months and 1.8 months, respectively (hazard ratio, 0.61, adjusted for stratification categories; P<0.001). OS was 6.7 months and 4.7 months, respectively (HR, 0.70; P<0.001), in favor of Tarceva(26).
3. Erlotinib is recommended by NCCN (but it is not FDA approved so the package insert does not include this indication) for NSCLC patients with EGFR mutations. In a pivotal phase III trial study (EURTAC) 1227 patients were screened for mutations and 174 were found to have mutations and were randomized to receive erlotinib vs platinumbased CT. PFS in the erlotinib arm was 9.4 months (HR, 0.42; P<0.0001), compared to 5.2 months (95%CI, 4.45.8 m) in the CT arm. Median OS, not statistically significant, was 22.9 months in the erlotinib arm and 18.8 months in the CT arm (HR, 0.80; P=0.42)(27).
Cost per month ranges from $4688.87(30 tabs of 100 mg) to $6535.04 (30 tabs of 150 mg). The dose used in pancreatic cancer is 100 mg once a day and in NSCLC is 150 mg once a day.
14. Axitinib (Inlyta)Axitinib has been FDA approved in January 2012 for
the treatment of advanced renal cell carcinoma, in patients in which other agents have not been effective. This approval was based on the AXIS phase III trial that included 723 patients with metastatic clear cell RCC who were randomly assigned to treatment with either axitinib (5 mg twice a day) or sorafenib (400 mg twice a day)(10). This study found a significant improvement in PFS (7 versus 5 months, HR for PFS, 0.67, 95% CI 0.540.81). The benefit in PFS was higher in patients previously treated with cytokines (median 12 versus 7 months, HR 0.46, 95% CI 0.320.68) than in patients previously treated with sunitinib (median 5 versus 3 months, HR 0.74, 95% CI 0.570.96)(10).
The recommended dose is 5mg po bid. One1mg tablet cost is $22. One 5 mg tablet cost is $165. The cost per month using 1 mg tabs is $6600 and using 5 mg tabs is $9900.
15. Bevacizumab (Avastin)Bevacizumab is an antivascular endothelial growth
factor (VEGF) monoclonal antibody that is FDA approved since February 2004 for front line and since June 2006 for second line in the treatment of metastatic colorectal cancer in combination with chemotherapy. It is also approved since October 2006 as front line treatment of nonsquamous lung cancer, in combination with chemotherapy. In May 2009, bevacizumab is also approved for the second line treatment of grade 3 and grade 4 malignant gliomas. Also, since August 2009 bevacizumab was approved for metastatic renal cell cancer.
In patients with metastatic colorectal cancer, in a pivotal early trial, the addition of bevacizumab to the bolus irinotecan/5 FU/leucovorin (IFL) regimen significantly improved response rates (45 versus 35 percent, P=0.004)), PFS (10.6 versus 6.2 months, HR for disease progression, 0.54; P<0.001), and OS (20.3 versus 15.6 months, HR for death of 0.66 (P<0.001)(53). In 2004, the Intergroup N9741 trial(54) showed a significant improvement in OS in patients treated with FOLFOX versus bolus IFL and since then FOLFOX became the standard of care frontline treatment of patients with metastatic colorectal cancer. To date, there are still only limited data on the benefit of adding bevacizumab to an oxaliplatinbased regimen in frontline treatment of metastatic colorectal cancer but, despite the lack of data, the majority of oncologists in US use the FOLFOX+bevacizumab combination in this setting. In fact, a large randomized Phase III study, that used a 2 x 2 factorial design and investigated the benefit of adding bevacizumab versus placebo to XELOX or FOLFOX4 did not show any improvement in survival using bevacizumab. A total of 1,401 patients were randomly assigned in this 2 x 2 analysis. Median PFS was 9.4 months in the bevacizumab arm and 8 months in the placebo arm (HR, 0.83; 97.5% CI, 0.72 to 0.95; P = 0.0023). Median OS was 21.3 months in the bevacizumab arm and 19.9 months in the placebo arm, but these results were not statistically significant. (HR, 0.89; 97.5% CI, 0.76 to 1.03; P =0 .077)(55). Interestingly, in the second line setting, adding bevacizumab to an oxaliplatin based regimen showed an improvement of both the OS (12.9 months compared with 10.8 months for the group treated with FOLFOX4 alone; HR for death = 0.75; P =0.0011) and in PFS (7.3 months, compared with 4.7 months for the group treated with FOLFOX4 alone HR for progression = 0.61; P <0.0001)(56).
Bevacizumab demonstrated significant clinical activity in second line treatement of grade 3 and grade 4 malignant gliomas both alone and in combination with irinotecan. The prognosis for recurrent malignant glioblastomas is gruesome, with median survivals of 3 to 9 months(57). Most of the data come from a noncomparative phase II trial, in which 167 patients with recurrent glioblastoma multiforme (GBM) were randomly assigned to bevacizumab (10 mg/kg), either as a single agent or at the same dose in conjunction with irinotecan (125 mg/m2 for those not taking enzymeinducing antiepileptic agents and 340 mg/m2 for those taking these agents). Treatment cycles were repeated every two weeks. The median OS time from the time of random assignment were 9.2 months (95.0% CI, 8.2 to 10.7 months) for the bevacizumab group and 8.7 months (95.0% CI, 7.8 to 10.9 months) for the bevacizumab+ CPT11 group. The estimated 6month PFS rates were 42.6% (97.5% CI, 29.6% to 55.5%) in the BV group and 50.3% (97.5% CI, 36.8% to 63.9%) in the bevacizumab + CPT11 group(58).
There are two randomized Phase III studies that established the benefit of Bevacizumab in the treatment of metastatic renal cell cancer. In the AVOREN study, 649 previously untreated patients were randomized to receive interferon alpha (IFNa, 9 million units three times per week for one year) plus either bevacizumab (10 mg/kg every two weeks) or placebo. PFS was significantly prolonged in the
www.revista-hipocrate.ro REZUMAT

Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România
Reclama

| Septembrie 201236
bevacizumab arm (10.2 versus 5.5 months, HR 0.63, 95% CI 0.450.72)(59), but the improvement in the OS was not statistically significant (median survival 23.3 versus 21.3 months, HR 0.86, 95% CI 0.721.04)(60). In a second Phase III study, 732 previously untreated patients with metastatic renal cell carcinoma were randomly assigned to either IFNalpha plus bevacizumab or IFNalpha plus placebo, on schedules similar to that used in the AVOREN trial. An interim analysis found that the PFS was significantly better in the patients receiving bevacizumab+IFNalpha: 8.5 months for patients receiving bevacizumab plus IFN (95% CI, 7.5 to 9.7 months) versus 5.2 months (95% CI, 3.1 to 5.6 months) for patients receiving IFN monotherapy (logrank P<.0001)(61). The median OS time was 18.3 months (95% CI, 16.5 to 22.5 months) for bevacizumab plus IFNalpha and 17.4 months (95% CI, 14.4 to 20.0 months) for IFNalpha monotherapy (unstratified logrank P = .097) which was not statistically significant. Adjusting on stratification factors, the hazard ratio was 0.86 (95% CI, 0.73 to 1.01; stratified logrank P = .069) favoring bevacizumab plus IFNalpha(62).
Initially, it has been shown that, for patients with NSCLC and good performance status, the addition of bevacizumab to the paclitaxel and carboplatin doublet improved the PFS and the OS, compared with chemotherapy alone. The median OS was 12.3 months in the group assigned to chemotherapy plus bevacizumab, as compared with 10.3 months in the chemotherapyalone group (HR for death, 0.79; P=0.003). The median PFS in the two groups was 6.2 and 4.5 months, respectively (hazard ratio for disease progression, 0.66; P<0.001), with corresponding response rates of 35% and 15% (P<0.001)(63). Subsequently, in a second randomized phase III trial of 1043 patients, the addition of bevacizumab to the cisplatin and gemcitabine doublet did not confirm a statistically significant effect on OS(64, 65).
Bevacizumab was also initially approved for metastatic breast cancer in February 2008, under the FDA’s accelerated approval program, which allows a drug to be approved based on data that are not sufficiently complete to permit full approval. On November 18, 2011, FDA revoked the agency’s accelerated approval of the breast cancer indication for Avastin manufactured by Genentech. Bevacizumab used for metastatic breast cancer has not been shown to provide a benefit, in terms of delay in the growth of tumors that would justify its serious and potentially lifethreatening risks. Nor was there enough evidence that use of bevacizumab will either help women with breast cancer live longer or improve their quality of life. In a pooled analysis of data for bevacizumab and firstline chemotherapy from E2100, AVADO, and RIBBON1, the addition of bevacizumab significantly improved median PFS (9.2 versus 6.7 months), but not OS (26.7 versus 26.4 months). Without an OS advantage, it is unclear whether the magnitude of improvement in PFS (2.5 months) is clinically meaningful, given the excess toxicity and expense of adding bevacizumab(23).
Cost. 100 mg/4ml cost $645.96, 400 mg/16 ml cost $2,525.85. Bevacizumab is approved at a dose of 5mg/kg or 10 mg/kg every 2 weeks for the treatment of metastatic colorectal cancer. The dose used in NSCLC, GBM and re
nal cell cancer is 10 mg/kg every 2 weeks.
16. Sorafenib (Nexavar)Sorafenib is a smallmolecule inhibitor of tyrosine ki
nases that is approved for the treatment of advanced renal cell carcinoma since December 2005 and since November 2007 for some cases of hepatocellular carcinoma. The activity of sorafenib in advanced RCC was demonstrated in the phase III TARGET trial, in which patients with advanced RCC who had failed prior standard therapy were randomly assigned to sorafenib (400 mg orally twice daily) or placebo. The median PFS was significantly longer in those receiving sorafenib compared with placebo (5.5 versus 2.8 months, HR 0.44, 95% CI 0.350.55). OS was not significantly prolonged compared to placebo (median 17.8 versus 15.2 months, HR 0.88, 95% CI 0.741.04). However, when postcrossover placebo survival data were censored, the difference became significant (17.8 v 14.3 months, respectively; HR = 0.78; P = .029)(34).
For liver cancer, the multicenter European SHARP trial randomly assigned patients with inoperable hepatocellular carcinoma and ChildPugh A cirrhosis to sorafenib or placebo. OS was significantly longer in the sorafenibtreated patients (10.7 versus 7.9 months), as was time to radiologic progression (5.5 versus 2.8 months)(35).
The monthly cost of treatment is $8377.13 (120 tabs of 200 mg). The approved daily dose of Nexavar is 400 mg twice a day.
17. Sunitinib (Sutent) Sunitinib is another smallmolecule tyrosine kinase in
hibitor that is approved since January 2006 for the treatment of patients with metastatic renal cell carcinoma. It is also approved since May 2007 for the treatment of gastrointestinal stromal tumors (GIST) that are not responding to imatinib, and since May 2011 for the treatment of pancreatic neuroendocrine tumors that cannot be removed by surgery, are locally advanced, or have metastasized.
Sunitinib was evaluated in a phase III trial with largely good or intermediateprognosis metastatic clear cell RCC who had not received prior systemic therapy. Median PFS was significantly prolonged (11 versus 5 months, HR 0.54). OS was also prolonged with sunitinib (median 26.4 versus 21.8 months, HR0.82, 95% CI 0.671.00, p=0.051)(6, 7, 31).
An international phase III trial of sunitinib versus placebo in 312 patients with refractory GIST established the role of sunitinib in this setting. 312 patients were randomized in a 2:1 ratio to receive sunitinib (n=207) or placebo (n=105); the trial was unblinded early when a planned interim analysis showed significantly longer time to tumor progression with sunitinib. The duration of PFS was clearly in favor of sunitinib: median PFS was 24.1 weeks (95% CI 11.1–28.3) for sunitinib, 6.0 weeks (4.4–9.9) for placebo, respectively (HR 0.33; 95% CI, 0.24–0.47; p<0.0001). OS obtained with initial sunitinib treatment was better than the one obtained with placebo, despite the option to cross over (HR 0.49, 95% CI 0.29–0.83; p=0.007). The authors stated that, since more than half the patients in the sunitinib group were still alive at the time of the interim analysis, a median OS value could not be calculated(52).
www.revista-hipocrate.ro REZUMAT

Septembrie 2012 | 37
Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România
Reclama

| Septembrie 201238
Sunitinib was also studied in patients with advanced, welldifferentiated pancreatic neuroendocrine tumors in a phase III multinational randomized, doubleblind, placebocontrolled study. 171 patients were randomly assigned to receive either sunitinib at a dose of 37.5 mg per day or placebo. Median PFS was 11.4 months in the sunitinib arm as compared with 5.5 months in the placebo arm (HR for progression or death, 0.42; 95% CI, 0.26 to 0.66; P<0.001). Nine deaths were reported in the sunitinib arm (10%) and 21 deaths were reported in the placebo group (25%) and most patients were still in followup at the data cut off point. The hazard ratio for death was 0.41 (95% CI, 0.19 to 0.89; P = 0.02) in favor of sunitinib. The authors stated that, due to the relatively high number of censored events, median OS could not be estimated for either study group(51).
The approved daily dose for renal cell carcinoma and GIST is 50 mg/day and the dose for pancreatic neuroendocrine tumors (PNET) is 37.5 mg/day. Costs are: 12.5 mg (28 tabs) $2596.10; 25 mg (28) $5508.22; 50 mg (28 tabs) $10465.92. The monthy cost of treatment ranges from 8100 (PNET) to 10,465.92 (renal cell cancer and GIST).
18. Pazopanib (Votrient)Pazopanib is FDA approved since January 2012 to
treat patients with advanced renal cell carcinoma and since March 2012 to treat advanced soft tissue sarcoma. In a phase III trial, patients, patients who were previously untreated or had received only cytokine therapy, were randomly assigned to Votrient or placebo. There was a significant increase in PFS with Votrient compared with placebo (median 9.2 versus 4.2 months, HR 0.46, 95% CI 0.340.62), with significant increases both in previously untreated patients and in those who had received cytokine therapy(32). Almost all patients had good or intermediate risk. In the final analysis of the study presented in 2010 at ESMO, H.R. 0.91, CI 0.711.16) the increase in OS was nonsignificant. (median OS of 22.9 versus 20.5 months). The authors’ impression was that the final analysis of OS was confounded by the early, frequent, and prolonged crossover to Votrient from patients originally randomized to placebo(33).
Pazopanib has also activity in advanced nonadipocytic softtissue sarcoma. An international Phase III study was conducted in 13 countries and 369 patients were randomly assigned in a 2:1 ration to receive pazopanib or placebo. Median PFS was 4.6 months (95% CI 3.7—4.8) for pazopanib compared with 1.6 months (0.9—1.8) for placebo (HR 0.31, 95% CI 0.24—0·40; p<0.0001). OS was 12.5 months (10.6—14.8) with pazopanib versus 10.7 months (8.7—12.8) with placebo, but this was not statistically significant (HR 0.86, 0.67—1.11; p=0.25)(87).
The recommend daily dose is 800 mg once a day. The cost per month using 120 tabs of 200 mg tabs is $6250.64.
19. Ipilimumab (Yervoy)Ipilimumab is FDA approved since March 2011 to
treat patients with unresectable or metastatic melanoma. This monoclonal antibody is directed against cytotoxic Tlymphocyteassociated antigen4 (CTLA4), which is expressed on the surface of activated T cells as part of a “checkpoint” to prevent a runaway immune respon
se. By inhibiting CTLA4, ipilimumab stimulates the immune system to attack melanoma cells. There were two Phase III studies that established the benefit of ipilimumab in the treatment of metastatic melanoma. In a placebo controlled, Phase III trial, 676 patients were randomly assigned in a 3:1:1 ratio to ipilimumab plus a glycoprotein 100 (GP100) vaccine, ipilimumab alone, or GP100 alone. All patients were HLAA0201 positive and had unresectable metastatic melanoma. All patients had received prior systemic treatment for advanced disease with either cytotoxic chemotherapy or interleukin2. OS was significantly increased in the two groups that received ipilimumab (median 10.0 and 10.1 versus 6.4 months, in the ipilimumab plus gp100, ipilimumab alone, and gp100 groups, hazard ratio (HR) for death 0.68 and 0.66 versus gp100 alone, respectively). OS rates for the three groups were 44, 46, and 25% at 12 months and 22, 24, and 14% at 24 months, respectively. The PFS in the three groups was the same. The median PFS was 2.76 months (95% CI, 2.73 to 2.79) in the ipilimumabplus gp100group, 2.86 months (95% CI, 2.76 to 3.02) in the ipilimumabalone group, and 2.76 months (95% CI, 2.73 to 2.83) in the gp100alone group.(48) In the second study, 502 patients with previously untreated metastatic melanoma, were randomized in a 1:1 ratio, to ipilimumab (10 mg per kilogram) plus dacarbazine (850 mg per square meter of bodysurface area) or dacarbazine (850 mg per square meter) plus placebo, given at weeks 1, 4, 7, and 10, followed by dacarbazine alone every 3 weeks through week 22. The median OS in the ipilimumab–dacarbazine group was 11.2 months (95% CI, 9.4 to 13.6), as compared with 9.1 months (95% CI, 7.8 to 10.5) in the dacarbazine group, with estimated survival rates in the two groups, respectively, of 47.3% and 36.3% at 1 year, 28.5% and17.9% at 2 years, and 20.8% and 12.2% at 3 years (HR for death with ipilimumabdacarbazine, 0.72; P<0.001). There was a 24% reduction in the risk of progression in the ipilimumabdacarbazine group as compared with the dacarbazine group (HR for progression, 0.76; P =0.006). The median values for PFS were similar. The authors interpreted this lack of difference in PFS as a result of a too early first assessment done at 12 weeks; after the first assessment the Kaplan Meier curves separated(49).
The approved dose is 3 mg/kg every 3 weeks for 4 doses. The cost of 50 mg is $6000. The total cost of an ipilimumab treatment is approximately $100,000.20. Sipoleucel T (Provenge)
Sipoleucel T is FDA approved since April 2010 for the treatment of asymptomatic or minimally symptomatic patients with metastatic hormonerefractory prostate cancer patients. Two Phase II trials failed to demonstrate an improvement in PFS but showed a nonstatistically significant improvement in the OS (23.2 versus 18.9 months, HR 1.50, 95% CI 1.102.05)(46). OS was the primary endpoint in the phase III IMPACT trial that enrolled 512 men. At a median followup of 34 months, patients assigned to the sipuleucelT therapeutic vaccine had a statistically significant 4.1 month improvement in median OS (25.8 versus 21.7 months). Differences in OS could not be accounted for by variations in subsequent treatments. As in the phase II tri
www.revista-hipocrate.ro REZUMAT

als, PFS was not significantly prolonged (14.6 versus 14.4 weeks)(47). Per one dose that contains more than 50 million autologous CD54 cell activated with PAPGMCSF the cost is $31.000. Doses are administered at ~ 2 weeks interval for a total of 3 doses.
The total cost of a sipoleucel T treatment is $93.000.It is clear that, for certain cancer types, the treatment
with biological targeted agents represents a progress. For example, since its approval in US in 1998, trastuzumab has revolutionized the management of Her 2positive breast cancer, specifically in the subset of patients whose tumors express the human epidermal growth factor receptor
(HER)2 protein. According to observational data, the use of trastuzumab has reversed the worse prognosis associated with HER2positive status in women with breast cancer. In a multivariate analysis published in 2010, trastuzumab recipients with Her2positive disease had a 44% reduction in the risk of death, versus women with Her2negative disease (HR 0.56; 95% CI, 0.45 to 0.69; P < 0.0001)(82).
Currently, there are several biological targeted agents available for the treatment of metastatic renal cell cancer (mRCC). Despite the recent advances of the treatment for this disease, very recently, two world experts in mRCC made a sobering statement about the therapeutic progress
Commercial nameType of cancer in which the agent is FDA approved
Improvement of OS Improvement of PFSAverage cost for 4 months of treatment in US
HerceptinAdjuvant Breast Yes YesMetastatic Breast Yes (5 mt) Yes Gastric Yes (3 mt) Yes $23,400
GleevecAdjuvant GIST No Yes Metastatic GIST Yes(~30mt) Yes $24,000
Erbitux
CR + Irinotecan refractory No Yes (2.6 mt)CR + FOLFIRI frontline Yes (3.5 mt) Yes (1.5 mt)Adjuvant H&N+RT Yes (20 mt) Yes (10 mt)Metastatic H&N +chemo Yes (3 mt) Yes (2.3 mt)Metastatic H&N alone N/A N/A $40,000
Vectibix Colorectal No Yes (1 mt) $42,400 Torisel Renal Yes (3.6 mt) Yes (2.3 mt) $21,500
Afinitor
Renal No Yes (3 mt)PNET No Yes (6.4 mt)SEGA N/A N/ABreast No Yes (4.2 mt) $32,000
Caprelsa Thyroid No Yes (11 mt) $23,400 Zelboraf Melanoma Yes Yes (4mt) $43,000 Xalkori Lung+ALK rearrangement N/A N/A $41,200 Perjeta Breast No Yes (7mt) $22,800 Tykerb Breast No Yes (4 mt) $13,200 Iressa Lung (EGFR mut) NCCN end No Yes (3 mt) $7,200
Tarceva
Pancreatic Yes (2 wk) Yes (2 wk)Lung (maintenance) Yes (1 mt) Yes (1 wk)Lung (2d and 3d line) Yes (2 wk) Yes (2 mt)Lung (EGFR mut) NCCN end No Yes (4.2 mt) $18,700-26,100
Inlyta Renal No Yes ( 2mt) $26,400
Avastin
CR met front+non-oxali chem. Yes (4.7mt) Yes (4.4mt)CR met front +oxali chem. No Yes (1.4 mt)CR met sec +oxali chem. Yes (2.1 mt) Yes (2.6 mt)Lung/nonsquamous +CarTax Yes (2 mt) Yes (1.7 mt)Lung/nonsquamous +CisGem No Yes (2wk)Brain N/A N/ARenal No Yes (4.7 mt) $20,200-40,400
NexavarLiver Yes (3 mt) Yes (2.7 mt)Renal No Yes (2.7 mt) $33,500
SutentPNET Yes Yes (6 mt)GIST Yes Yes (4.5mt)Renal Yes (4.6 mt) Yes (6 mt) $32,400-41,800
VotrientSoft Tissue Sarcoma No Yes (3 mt)Renal No Yes (5 mt) $25,000
Yervoy Melanoma Yes (3.5 mt) No $100,000 Provenge Prostate Yes (4.1 mt) No $93,000 GIST=gastrointestinal stromal tumor; DFSP=dermatofibrosarcoma protuberans; PNET= pancreatic neuroendocrine tumors; SEGA=subepenymal giant cell astrocytoma; N/A=data not available, no Phase III studies reported; PFS=progression free survival; OS=overall survival; mt=months, wk=weeks; CR=colorectal cancer; met=metastatic; oxali=oxaliplatin; mut=mutated; CarTax=Carboplatin/Taxol; CisGm=Cisplatin/Gemcitabine NCCN end=NCCN endorsed (not FDA approved).
Septembrie 2012 | 39
Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România

| Septembrie 201240
in this disease: “despite advances in treatment, most patients with advanced disease still face a dramatically shorted life expectancy. An objective look at the therapeutic landscape shows development of only two classes of agents, after an expenditure of billions of dollars and involvement of thousands of patients in clinical trials, with little or no effort to understand the determinants of response and resistance”(8).
For many cancer types, the benefit of biological targeted agents appears to be borderline and the treatment is prohibitively expensive. As shown above, there is no OS proven benefit of cetuximab in second or third line in refractory metastatic colorectal cancer and the price of administering cetuximab weekly for one at 250 mg/m2 is $120,000. In a clinical setting like this, when the proven benefit is so small and the treatment is so expensive, should we mention this therapeutic option to patients that can not afford paying for the drug? Similar questions pose serious ethical dilemmas.
What can be done? The regulating agencies play a key role in establishing the standards of care for cancer patients. The medical community should also share some responsibility and be proactive in discussing the clinical aspects of these issues. The withdrawal by the FDA of the indication of bevacizumab in metastatic breast cancer, for example, raises fundamental clinical questions about the validity of the PFS as an endpoint, especially when the OS is not affected and the improvement in PFS is doubled by questionable amelioration of quality of life and potentially lifethreatening side effects. Some authors advocate the use of OS as the gold standard marker for efficacy and consider PFS a measure of a drug effect while administered and not a surrogate for overall survival(84,85). Other authors argue that the measurement of OS typically requires a long followup period, a large population to ensure significant differences between the study groups and is vulnerable to the confounding effects of subsequent therapy and crossover(86). It is possible that both positions may be right in different clinical settings. For certain tumors (e.g. metastatic ovarian cancer or metastatic renal cell carcinoma), PFS may represent a valid surrogate point for OS while, in other (e.g. metastatic melanoma or metastatic prostate cancer), OS should be used. It is also important to recognize that, due to their specific mechanisms of actions, some of the new agents (Ipilimumab or Sipoleucel T, for example) may improve the OS without affecting the PFS(47, 49).
Few months ago, the American Society of Clinical Oncology has published its top five “DO NOT” list for oncology(5):
1. Don’t use cancerdirected therapy for solid tumor patients with the following characteristics: low performance status (3 or 4), no benefit from prior evidencebased interventions, not eligible for a clinical trial, and no strong evidence supporting the clinical value of further anticancer treatment.
2. Don’t perform PET, CT and radionuclide bone scans in the staging of early prostate cancer at low risk for metastasis.
3. Don’t perform PET, CT and radionuclide bone scans in the staging of early breast cancer at low risk for metastasis.
4. Don’t perform surveillance testing (biomarkers) or imaging (PET, CT and radionuclide bone scans) for asymptomatic individuals who have been treated for breast cancer with curative intent.
5. Don’t use white cell stimulating factors for primary prevention of febrile neutropenia for patients with less than 20% risk for this complication.
Specific guidelines to reduce unnecessary costs of using biological target agents have also been suggested. Here are some of them:
FDAapproved should be strictly adhered to and extrapolations should be avoided. For example, a drug approved for first line treatment should not be used in second or third line treatment if it is not approved for that indication. There are, of course, exceptions to this rules, but this are very few. For example, although not FDA approved for this indication, erlotinib and gefitinib are endorsed by NCCN for use in patients with lung cancer that bear EGFR mutations. In US, the endorsement of a drug by a nationally recognized group like NCCN is considered by the insurance companies and the practitioners a surrogate for FDA approval.
Drugs shown to be active in one subset of patients should be prescribed for that subset only.
Cheaper alternate chemotherapy regimens should be offered, if available.
Side effects and quality of life should be taken into consideration, especially when the biological targeted treatment offers only marginal benefit(81).
Ideally, in order to optimize costeffectiveness, biological targeted agents should rise to the promise of their name and be used only in patients with tumors expressing the relevant molecular target. Standardized and reliable means of measuring the target should be made available before blindly using new drugs. A retrospective analysis published in June 2011 in the Journal of Clinical Oncology supported the idea that molecular targeted agents produced the highest relative benefit when the target population was selected by a biomarker(83). However, in practice, the priorities and rationales of drug marketing are different from those of scientific research. The development of biomarkers is a laborious and costly process. “Marketing departments in the pharmaceutical industry tend to favor ‘organ’based drug registrations, while scientific data increasingly suggest that only those that express the relevant biomarker target will benefit from the treatment”(80).
The treatment of cancer evolves very fast and almost every month new drugs or new indications are approved. This overview of twenty currently approved biological targeted agents in solid tumors is just a snapshot of the situation in August 2012 and most likely it will become quickly outdated. Recently, HemOnc today published a list of more than 430 oncology drugs currently in the pipeline(79). How many of these agents are going to be proven to be beneficial and at what price?
Doru Paul, MD has no conflicts of interest.
www.revista-hipocrate.ro REZUMAT

BIBLIOGRAFIESawyers C. Targeted cancer therapy. Nature, 2004, 432: 294-298.Thatcher N. Chang A, Parikh P, et al: Gefitinib plus best supportive care in previously treated patients with refractory advanced non-small-cell lung cancer: Results from a randomized, placebo-controlled, multicentre study (Iressa Survival Evaluation in Lung Cancer). Lancet, 2005; 366:1527-1537.http://www.accessdata.fda.gov/scripts/cder/drugsatfda/http://www.drugstore.comLowell E. Schnipper, Thomas J. Smith, Derek Raghavan, Douglas W. Blayney, Patricia A. Ganz, Therese Marie Mulvey, and Dana S. Wollins. American Society of Clinical Oncology Identifies Five Key Opportunities to Improve Care and Reduce Costs: The Top Five List for Oncology. JCO May 10, 2012:1715-1724.Figlin RA, Hutson TE, Tomvzak P, et al. Overall survival with Sunitinib versus interferon (IFN)-alfa as first-line treatment of metastatic renal cell carcinoma (mRCC). JCO August 18, 2008; 26 (Suppl); Abstract 5024.Motzer RJ, Hutson TE, Tomczak P, et al. Sunitinib versus Interferon alfa in metastatic renal cell carcinoma. NEJM 2007; 356: 115-124.Jonasch E and Motzer RJ. Ten years of progress in Renal Cell Carcinoma. JNCCN, June 2012 Vol. 10, Number 6: 690-693.Motzer RJ, Escudier B, Oudard S, et al. Efficacy of everolimus in advanced renal cell carcinoma; a double blind, randomised, placebo controlled phase III trial. Lancet 2008; 372; 449-456.Rini BI, Esxcudier B, Tomczak P, et al. Comparative effectiveness of Axitinib versus Sorafenib in advanced renal cell carcinoma (AXIS); a randomized phase 3 trial. Lancet 2012; 378: 1931-1939.Kantarjian H, et al. Very long-term follow-up results of imatinib mesylate therapy in chronic phase chronic myeloid leukemia after failure of interferon alpha therapy. Cancer 15 June 2012, Vol. 118; Issue 12: 3116–3122.Fojo T, Parkinson DR. Biologically targeted cancer therapy and marginal benefits: Are we making too much of too little or are we achieving too little by giving too much? Clin Cancer Res, 2010 16:5972-5980.Weisenberg E, et al. Second generation inhibitors of BCR-ABL for the treatment of imatinib-resistant chronic myeloid leukaemia. Nature Reviews Cancer 7, 345-356 (May 2007).Sjoblom T, et al. The Consensus Coding Sequences of Human Breast and Colorectal Cancers Science, Vol. 314 no. 5797 pp. 268-274, September 7, 2006.The Cancer Genome Atlas Research Network Nature Vol 455, September 4 (2008).DeMatteo RP et al. Placebo-Controlled Randomized Trial of Adjuvant Imatinib Mesylate Following the Resection of Localized, Primary Gastrointestinal Stromal Tumor (GIST). Lancet. 2009 March 28; 373(9669): 1097–1104.Demetri GD, et al. Efficacy and Safety of Imatinib Mesylate in Advanced Gastrointestinal Stromal Tumors. NEJM, August 15, 2002, Vol. 347, No. 7.472-480.Blanke CD, et al. Phase III randomized, intergroup trial assessing imatinib mesylate at two dose levels in patients with unresectable or metastatic gastrointestinal stromal tumors expressing the kit receptor tyrosine kinase: S0033. J Clin Oncol. 2008 Feb 1;26(4):626-32.Slamon DJ, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. NEJM. 2001; 344(11):783-792.Edward HR, et al. Trastuzumab plus adjuvant Chemotherapy for Operable Her 2-Positive Breast Cancer. NEJM. 2005; 353(16):1673-1684.Moja L, et al. Trastuzumab containing regimens for early breast cancer. Cochrane Database Syst Rev. 2012;4: CD006243.Bang YJ, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet. 2010; 376(9742):687-697.O’Shaughnessy J, et al. A meta-analysis of overall survival data from three randomized trials of bevacizumab (BV) and first-line chemotherapy as treatment for patients with metastatic breast cancer (MBC). J Clin Oncol. 2010; 28:7s (abstract# 1005).Fukukoa M, et al. Biomarker Analyses and Final Overall Survival Results From a Phase III, Randomized, Open-Label, First-Line Study of Gefitinib Versus Carboplatin/Paclitaxel in Clinically Selected Patients With Advanced Non–Small-Cell Lung Cancer in Asia (IPASS). Journal of Clin Oncol. Jul 20, 2011:2866-2874.
Cappuzzo F, et al. Erlotinib as maintenance treatment in advanced non-small-cell lung cancer: a multicenter, randomised, placebo-controlled phase 3 study. Lancet Oncology June 2010, Vol. 11, 521-529.Shepherd LA, et al. Erlotinib in previously treated non-small-cell lung cancer. NEJM. 2005; 353(2):123-132.Rosell R, et al. Erlotinib versus chemotherapy (CT) in advanced non-small cell lung cancer (NSCLC) patients (p) with epidermal growth factor receptor (EGFR) mutations: Interim results of the European Erlotinib Versus Chemotherapy (EURTAC) phase III randomized trial. J Clin Oncol 29: 2011 (suppl; abstr 7503).Moore MJ, et al. Erlotinib plus Gemcitabine compared with Gemcitabine alone in patients with advanced pancreatic cancer: a phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol. 2007;25(15):1960-1966.Geyer CE, et al. Lapatinib plus Capecitabine for HER2-Positive Advanced Breast Cancer. NEJM. 2006; 355(26):2733-2743.Cameron D et al. Lapatinib plus Capecitabine in women with HER-2-positive advanced breast cancer: final survival analysis of a phase III randomized trial. Oncologist. 2010; 15(9):924-34.Motzer RJ et al. Overall survival and updated results for sunitinib compared with interferon alfa in patients with metastatic renal cell carcinoma. J Clin Oncol. 2009;27(22):3584-3590.Sternberg CN, et al. Pazopanib in locally advanced or metastatic renal cell carcinoma: results of a randomized phase III trial. J Clin Oncol. 2010; 28(6):1061.Sternberg CN, Hawkins RE, Szczylik C, et al. Randomized, double-blind phase III study of Pazopanib in patients with advanced/metastatic renal cell carcinoma: Final overall survival results (abstract # LBA22). Ann Oncol 2010; 21: (Supplement 8): viii1–viii12.Escudier B, et al. Sorafenib for treatment of renal cell carcinoma: Final efficacy and safety results of the phase III treatment approaches in renal cancer global evaluation trial. J Clin Oncol. 2009; 27(20):3312-3318.Llovet JM, et al. Sorafenib in advanced hepatocellular carcinoma. NEJM. 2008;359 (4):378-390.Hortobagyi GN, Piccart M, Rugo H, et al. S3-7: Everolimus for Postmenopausal Women with Advanced Breast Cancer: Updated Results of the BOLERO-2 Phase III Trial. Cancer Research: December 15, 2011; Vol. 71, Issue 24, Supplement 3.Hudes G, et al. Temsirolimus, interferon alfa, or both for advanced renal-cell carcinoma. NEJM. 2007; 356(22):2271-2281.Motzer RJ, Escudier B, Oudard S et al. Phase 3 trial of everolimus for metastatic renal cell carcinoma: final results and analysis of prognostic factors. Cancer. 2010; 116(18):4256-4265.Yao JC et al. Everolimus for Advanced Pancreatic Neuroendocrine Tumors. NEJM 2011; 364:514-523.Krueger DA, et al. Everolimus for subependymal giant-cell astrocytomas in tuberous sclerosis. NEJM. 2010 Nov 4; 363(19):1801-11.Wells SA, et al. Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer: a randomized, double-blind phase III trial. J Clin Oncol. 2012 Jan 10; 30 (2):134-41.Chapman PB, et al. Improved Survival with Vemurafenib in Melanoma with BRAF V600E Mutation. NEJM 2011; 364:2507-2516. http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/202570s003lbl.pdf.Shaw AT et al, Effect of crizotinib on overall survival in patients with advanced non-small-cell lung cancer harbouring ALK gene rearrangement: a retrospective analysis. Lancet Oncol. 2011; 12(11):1004-1012.Van Cutsem E, et al. Open-label phase III trial of panitumumab plus best supportive care compared with best supportive care alone in patients with chemotherapy-refractory metastatic colorectal cancer. J Clin Oncol. 2007; 25(13):1658-1664.Higano CS, Schellhammer PF, Small EJ, Burch PA, Nemunaitis J, Yuh L, Provost N, Frohlich MW. Integrated data from 2 randomized, double-blind, placebo-controlled, phase 3 trials of active cellular immunotherapy with sipuleucel-T in advanced prostate cancer. Cancer. 2009; 115(16):3670-3679.Kantoff PW, Higano CS, Shore ND et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. NEJM. 2010; 363(5):411-422.Hodi FS, et al. Improved survival with ipilimumab in patients with metastatic melanoma. NEJM. 2010; 363(8):711-723.Robert C, et al. Ipilimumab plus dacarbazine for previously
untreated metastatic melanoma. NEJM. 2011; 364(26):2517-2526.Baselga J, Cortés J, Kim SB, Im SA, Hegg R, Im YH, Roman L, Pedrini JL, Pienkowski T, Knott A, Clark E, Benyunes MC, Ross G, Swain SM. CLEOPATRA Study Group. Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer. NEJM. 2012 Jan; 366(2):109-119.Raymond E, et al. Sunitinib Malate for the Treatment of Pancreatic Neuroendocrine Tumors. NEJM. 2011; 364:501-513.Demetri GD, et al. Efficacy and safety of sunitinib in patients with advanced gastrointestinal stromal tumour after failure of imatinib: a randomised controlled trial. Lancet. 2006;368(9544):1329-1338.Hurwitz H, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. NEJM. 2004; 350(23):2335-2342.Goldberg RM, et al. A randomized controlled trial of fluorouracil plus leucovorin, irinotecan, and oxaliplatin combinations in patients with previously untreated metastatic colorectal cancer. J Clin Oncol. 2004; 22(1):23-30.Saltz LB, et al. Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III study. J Clin Oncol. 2008; 26(12):2013-2019.Giantonio BJ, Catalano PJ, Meropol NJ, O’Dwyer PJ, Mitchell EP, Alberts SR, Schwartz MA, Benson AB 3rd. Eastern Cooperative Oncology Group Study E3200. Bevacizumab in combination with oxaliplatin, fluorouracil, and leucovorin (FOLFOX4) for previously treated metastatic colorectal cancer: results from the Eastern Cooperative Oncology Group Study E3200. J Clin Oncol. 2007; 25(12):1539-1544.Wong ET, Hess KR, Gleason MJ, et al. Outcomes and prognostic factors in recurrent glioma patients enrolled onto phase II clinical trials. J Clin Oncol 1999;17: 2572–2578.Friedman HS, et al. Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol. 2009; 27(28):4733-4740.Escudier B, et al. Bevacizumab plus interferon alfa-2a for treatment of metastatic renal cell carcinoma: a randomised, double-blind phase III trial. Lancet. 2007; 370(9605):2103-2111.Escudier B, et al. Phase III trial of bevacizumab plus interferon alfa-2a in patients with metastatic renal cell carcinoma (AVOREN): final analysis of overall survival. J Clin Oncol. 2010; 28(13):2144-2150.Rini BI, et al. Bevacizumab plus interferon alfa compared with interferon alfa monotherapy in patients with metastatic renal cell carcinoma: CALGB 90206. J Clin Oncol. 2008; 26(33):5422-5428.Rini BI, et al. Phase III trial of bevacizumab plus interferon alfa versus interferon alfa monotherapy in patients with metastatic renal cell carcinoma: final results of CALGB 90206. J Clin Oncol. 2010; 28(13):2137-2143.Sandler A, Gray R, Perry MC, Brahmer J, Schiller JH, Dowlati A, Lilenbaum R, Johnson DH. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med. 2006; 355(24):2542-2550.Reck M, von Pawel J, Zatloukal P, Ramlau R, Gorbounova V, Hirsh V, Leighl N, Mezger J, Archer V, Moore N, Manegold C. Phase III trial of cisplatin plus gemcitabine with either placebo or bevacizumab as first-line therapy for nonsquamous non-small-cell lung cancer: AVAil. J Clin Oncol. 2009; 27(8):1227-1234.Reck M, von Pawel J, Zatloukal P, Ramlau R, Gorbounova V, Hirsh V, Leighl N, Mezger J, Archer V, Moore N, Manegold C, BO17704 Study Group. Overall survival with cisplatin-gemcitabine and bevacizumab or placebo as first-line therapy for nonsquamous non-small-cell lung cancer: results from a randomised phase III trial (AVAiL). Ann Oncol. 2010; 21(9):1804-1809.Van Cutsem E, et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. NEJM 2009; 360(14):1408-1417.Van Cutsem E, et al. Cetuximab plus irinotecan, fluorouracil, and leucovorin as first-line treatment for metastatic colorectal cancer: updated analysis of overall survival according to tumor KRAS and BRAF mutation status. J Clin Oncol. 2011; 29(15):1-10.Bokemeyer C, et al. Fluorouracil, leucovorin, and oxaliplatin with and without cetuximab in the first-line treatment of metastatic colorectal cancer. J Clin Oncol. 2009; 27(5):663-671.Bokemeyer C, et al. KRAS status and efficacy of first-line treatment of patients with metastatic colorectal cancer (mCRC) with FOLFOX with or without cetuximab: The OPUS experience. J Clin Oncol 26: 2008 (May 20 suppl; abstr 4000).
Septembrie 2012 | 41
Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România

| Septembrie 201242
l Dr. Louise S. Wilkinson Director of South West London Breast Screening Service and Consultant Breast Radiologist, St. George’s Healthcare NHS Trust, London
Most women with breast cancer are diagnosed because of symptoms or following routine mammographic screening. The National Health Service Breast Screening Programme was set up in the early 1990s with a remit to screen women between the ages of 50 and 65 on a 3 yearly cycle. Emphasis was placed on careful monitoring of the service and rigorous data collection. The availability of data allows ongoing service improvement and open discussion about the benefit and harm of screening. Over 2.75 million women between the ages of 45 and 74 were invited for screening in 2009/10, 2.1 million women were screened and 16476 cancers were detected. Around one
third of all breast cancers in the UK are detected through screening(1).
Symptomatic breast services in the UK have also changed over the same time, in response to changing national strategies with a greater reliance on imaging and by mirroring improvements in the screening services. Data collection is now seen as the key to providing uniformly high quality services. In 2009, 48417 women and 371 men in the UK were diagnosed with breast cancer(2).
This lecture will discuss the organisation of both screening and symptomatic services in a large London hospital, addressing the challenges of service improvement in a time of financial constraint, and dealing with the need for earlier diagnosis while avoiding overtreatment.
l R. Pietrosanu, R. Mehta, H. Gay, L. WilkinsonSt. George’s Healthcare NHS Trust
DCIS being an essential screening diagnostic, as a result of the implementation of different National Health Breast Screening Programmes, the apparent incidence has significantly increased, in the last decade.
The purpose of this presentation is to show what and how common DCIS is, but also how to maximize its detection, make an accurate local staging, establish its relationship with invasive cancer and to point out the most important radiological features, as well as pathologicalradiological correlation of the different grades of DCIS.
Last, but not least, communication of the diagnostic to patients and the possibilities of treatment should be considered as a very important aspect.
The future of DCIS would probably consist in better prediction of risk, more widespread screening, increasing the diagnosis of high nuclear grade DCIS and starting trials with minimal treatment for low nuclear grade DCIS, as well as improving the technology
Breast Diagnostic Services in the UK the Challenges of Maintaining Quality, Improving Efficiency, Promoting
Early Diagnosis and Avoiding Overtreatment
DCIS: which path to follow?
REFERENCES:1. http://www.cancerscreening.nhs.uk/breastscreen/publications/2011review.html2. http://info.cancerresearchuk.org/cancerstats/types/breast/incidence/
REFERENCES:Radiologic-Pathologic Correlation of DCIS- Yamada et al, Radiographics 2010Surgical management of breast cancerPerceptions of DCIS among UK health professionals-Kennedy et al, The breast 2010www.cancerscreening.nhs.uk/beastscreen/publications/2011review.htmlDCIS Radiology and communicating the diagnosis- R. Given-Wilson 2012
www.revista-hipocrate.ro REZUMAT
Maughan T, et al. Identification of potentially responsive subsets when cetuximab is added to oxaliplatin-fluoropyrimidine chemotherapy (CT) in first-line advanced colorectal cancer (aCRC): Mature results of the MRC COIN trial. J Clin Oncol 28:15s, 2010 (suppl; abstr 3502).Tveit K, et al. Randomized phase III study of 5-fluorouracil/folinate/oxaliplatin given continuously or intermittently with or without cetuximab, as first-line treatment of metastatic colorectal cancer: The NORDIC VII study (NCT00145314), by the Nordic Colorectal Cancer Biomodulation Group. J Clin Oncol 29: 2011 (suppl 4; abstr 365).Vermorken JB, et al. Platinum-based chemotherapy plus cetuximab in head and neck cancer. NEJM. 2008; 359(11):1116.Vermorken JB, et al. Open-label, uncontrolled, multicenter phase II study to evaluate the efficacy and toxicity of cetuximab as a single agent in patients with recurrent and/or metastatic squamous cell carcinoma of the head and neck who failed to respond to platinum-based therapy. J Clin Oncol. 2007; 25(16):2171-2177.Bonner JA, et al. Radiotherapy plus cetuximab for squamous-cell carcinoma of the head and neck. NEJM. 2006; 354 (6):567-578.
Bonner JA, et al. Radiotherapy plus cetuximab for locoregionally advanced head and neck cancer: 5-year survival data from a phase 3 randomised trial, and relation between cetuximab-induced rash and survival. Lancet Oncol. 2010; 11(1):21-28.Cunningham D et al. Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. NEJM 2004:351:337-345.Voncken JW, Morris C, Pattengale P, Gunther D, Kikly C, Groffen J, and Nora Heisterkamp N. Clonal Development and Karyotype Evolution During Leukemogenesis of BCR/ABL Transgenic Mice. Blood, 1992, Vol. 79, No4:1029-1036.http://quickfacts.census.gov/qfd/states/00000.html.HemOnc Today Volume 13, Number 10, May 25 2012, Page 67-79.Soria JC., J. Y. Blay JY, Spano JP, Pivot X, Coscas Y and Khayat D. Added value of molecular targeted agents in oncology. Annals of Oncology Vol. 22, Issue 8:1703-1716.Fojo T and Grady C. How much is life worth: Cetuximab, Non-Small Cell Lung cancer and the $440 billion question. 2009, Vol. 101, Issue 15, 1044-1048.
Dawood S, et al. Prognosis of women with metastatic breast Cancer by HER2 status and Trastuzumab treatment: An institutional-based review. J Clin Oncol 2010, Vol.28, Number 1, 92-98.Amir E, et al. Oncogenic targets, magnitude of benefit, and market pricing of antineoplastic drugs. J Clin Oncol 2011, Vol. 29, Number 18:2543-2549.Driscoll JJ and Rixe O. Overall Survival: Still the Gold Standard Why Overall Survival Remains the Definitive End Point in Cancer Clinical Trials. The Cancer Journal, 2009, Vol .15, Number 5: 401-406. Wilkerson J and Fojo T. Progression-Free Survival is simply a measure of a drug’s effect while administered and is not a surrogate for overall survival. The Cancer Journal, 2009, Vol. 15, Number 5:379-385.Lebwohl D, Kay A, Berg W, Baladi JF, and Zheng J. Progression-Free Survival gaining on overall survival as a gold standard and accelerating drug development. The Cancer Journal, 2009, Vol.15, Number 5:386-394.van der Graaf, et al. Pazopanib for metastatic soft-tissue sarcoma (PALETTE): a randomised, double-blind, placebo-controlled phase 3 trial. The Lancet, 2012, Vol. 379, Issue 9829; 1879 – 1886.

l Dan Jinga MD PhD, Adina Croitoru MD PhD The Oncotype DX® Assay in the Contemporary Management of Invasive Earlystage Breast Cancer
The Recurrence Score® Result uses key genes linked to critical molecular pathways. The final gene set used for the Oncotype DX® assay includes the 16 cancer genes identified in the clinical trials: 5 genes are in the proliferation group, 2 in the HER2 group, 4 in the estrogenreceptor group, 2 in the invasion group, and 3 are unaligned. Some of the genes are well known in the breast cancer literature; others are relatively new. The 5 reference genes are used for normalizing the expression of the cancerrelated genes.
The Recurrence Score® Result assesses individual tumor biology for ER+ breast cancer. The Oncotype DX® Recurrence Score® is correlated with distant recurrence rate at 10 years, hormone therapy benefit, and chemotherapy benefit. There is a continuous biology of breast cancer that is revealed by the Recurrence Score. There are clear underlying phenotypes that correspond to low recurrence score disease and high recurrence score disease:
Distant recurrence rate at 10 years with 5 years of tamoxifen treatment: the higher the score, the higher the risk of distant recurrence;
Hormone therapy benefit: the lower the score, the greater the impact of tamoxifen given for 5 years on proportion of patients recurrencefree at 10 years;
Chemotherapy benefit: the higher the score, the greater the proportion of patients distant recurrencefree at 10 years.
The Oncotype DX® Assay identifies patients for whom tamoxifen alone may be appropriate therapy and, also can predict benefit from chemotherapy added to tamoxifen. The KaplanMeier estimates of the risk of death from breast cancer at 10 years indicate that systemic treatment with tamoxifen is more beneficial in low and intermediaterisk patients and the addition of chemotherapy to tamoxifen is more beneficial in highrisk patients.
Oncotype DX® Colon Cancer AssayThe Recurrence Score contains gene groups con
sistently identified in the 1851 patients from the development studies, and the validation of the Recurrence Score in QUASAR provides strong support for their biological relevance. The 12gene Recurrence Score includes 7 cancer genes and 5 reference genes. The 7 cancer
genes include the 2 key biologic pathways (cell cycle genes and stromal genes) identified as being associated with recurrence in the development studies, as well as an individual gene GADD45B (associated with cellular response to stress).
QUASAR Results:The validation study protocol specified secondary
analyses to characterize risk resolution across the range of Recurrence Score.
Protocolspecified cutpoints at 30 and 41 were used to separate the population into 3 groups of patients of sufficient size to enable statistical analyses.
KaplanMeier analysis of the 3 groups defined by the prespecified cutpoints demonstrates a separation of 3 year recurrence risk between the groups, with average risk in the low risk group of 12% and average risk in the high risk group of 22%.
Protocolspecified comparison of the high vs low recurrence risk groups in a Cox model shows significant HR 1.47 (with p<0.05)
It is important to note that the clinical utility of the assay resides in the continuous Recurrence Score, which provides individualized recurrence risk information over a range from 911% at the low end to 2527% at the high end. Our discussions with oncologists would suggest that thresholds for clinical actionability (i.e. the decision to recommend treatment or not) will depend on the individual patient’s clinical situation.
Protocol specified secondary analyses included univariate and multivariate analyses of clinical and pathologic covariates with RFI in Cox propor t ional h a z a r d s models. In univariate analyses, the clinical and pathologi cal covariates found to have the most significant relationship to recurrencefree interval
Septembrie 2012 | 43
Importance of OncotypeDX in breast and colorectal cancer
treatment planning
Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România

| Septembrie 201244
l Winald Gerritsen, MD, PHD
Prof dr. Winald Gerritsen is medical oncologist with a background in translational research with a special interest in tumor immunology and prostate cancer. Currently, he is leading the tumor immunology program for melanoma and prostate cancer at the Radboud University medical center in Nijmegen. He was director of Vumc Cancer Center Amsterdam.
Prof. Gerritsen has chaired the Dutch Society of Gene Therapy and became honorary member of the society. He has served as a chairman of the commission of clinical re
search of the Dutch Cancer Society (KWF). He chaired the commission of biotherapy of the National Translational Cancer Research Network, UK and is a member of the Cancer Research UK Immunotherapy Quinquennial Review Committee. He is also member of the Royal Holland Society of Sciences and Humanities and has a Adjunct professorship at John Hopkins University. Recently, he was visiting professor at Oxford University Cancer Center.
Following his medical training at the University of Nijmegen, Prof. Gerritsen achieved his PhD in 1989 on bone marrow transplantation at the Medical School of the Erasmus University of Rotterdam. From 1989 till 1991
Current Focus of Cancer Immunotherapy Improving Clinical Benefit and Prolonging Survival
www.revista-hipocrate.ro REZUMAT
Current Treatment of Bone Sarcomal Juergen Bruns Unit for orthopaedic surgery, AGAPLESIONDiakonieklinikum Hamburg
Bone sarcomas are rare primary malignant tumors and account for nearly 1% of all malignant tumors. While osteo and Ewing’s sarcomas are the most frequent sarcomas of all, with a peak incidence in the first two decades, the most often bone sarcomas in adults are the different types of chondrosarcomas.
Osteosarcomas occur most frequently in the knee region and in the hip region, less frequently in the pelvis and other long bone of the skeleton. Ewing’s sarcoma are located more often in the proximal femur, the pelvis and the ribs. Chondrosarcoma have a predominance in the proximal and distal femur, the pelvis and the long bone of the upper extremities. Socalled secondary sarcoma of bone occur after radiation for others reasons, following longlasting Paget’s disease, chondromas or giantcell tumors of the bone.
In most of these sarcomas, the treatment protocol includes pre and postoperative chemotherapy
(osteosarcoma and Ewing’s sarcoma and some rare entities) and/or additional radiotherapy (Ewing’s sarcoma). In order to ensure the optimal conditions for a recurrencefree survival in all patients, a wide resection is the treatment of choice.
In most of the cases, a wide resection is possible without amputation. There are several reconstructional procedures, such as megaprostheses or biological reconstructions using non or vascularized autologous bone such as fibulae. In rare cases, such as in the scapula, clavicle or fibula, simple resection of bone without reconstruction is possible. In recent years, the rate of rotational plasties is decreasing.
In order to achieve the main goal “wide resection”, sometimes additional reconstructional techniques, in cooperation with a plastic surgeon are necessary.
(RFI) were mismatch repair status (MMR) and Tstage (data not shown in this presentation). In a protocolspecified multivariate analysis, Recurrence Score remained significantly associated with RFI after simultaneously controlling for the prognostic effects of MMR, T stage, tumor grade, number of nodes examined, and LVI, with Recurrence Score retaining the HR and significance level observed in univariate analyses. In these multivariate analyses, three factors Recurrence Score, MMR status and T stage were found to be the most significant independent predictors of recurrence risk following surgery.
ConclusionAlthough the Recurrence Score will likely yield its hi
ghest value when used as a continuous measure, to obtain individualized estimates of recurrence risk, an analysis of the QUASAR data permits the identification of “guideposts” which may be useful for clinical decisionmaking. These guideposts have been identified on the basis of internal consistency within the data, and are not, in any manner, meant to be prescriptive – ultimately, decision making with an individual patient should be based on clinical judgment after review of the relevant clinical data, including Recurrence Score.

Septembrie 2012 | 45
l Delia Mateescu
Anul acesta, în ianuarie, sau împlinit 10 ani de când a fost aprobat de c`tre FDA pegfilgrastim (Neulasta® Amgen), pentru reducerea riscului neutropeniei febrile (FN) la pacien]i oncologici trata]i cu regimuri de chimioterapie agresive.
Introducerea acestui inovator factor de cre[tere a coloniilor de granulocite, dup` ce ini]ial compania Amgen lansase Filgrastim (Neupogen®), primul compus în clasa cu administrare zilnic`, a marcat un eveniment istoric de mare anvergur`, oferind oportunitatea de îmbun`t`]ire a complian]ei pacientului la tratament. Deriv` din filgrastim, îns` are ata[at` o grupare de polietilenglicol [PEG] care îi confer` o greutate molecular` mai mare, permi]ând moleculei s` persiste mai mult timp în organism. Cu alte cuvinte, este un compus cu ac]iune lung`, care î[i autoregleaz` metabolismul [i care se administreaz` o singur` dat` pe cura de chimioterapie. Se administreaz` la cel pu]in 24 de ore dup` chimioterapie,
dar nu mai devreme de 14 zile înaintea urm`torului ciclu de chimioterapie.
În trialurile clinice, pegfilgrastim a dovedit aceea[i eficacitate crescut` ca [i predecesorul lui [i aceea[i tolerabilitate excelent`. Întro metanaliz` recent` (Cooper KL et al. BMC Oncol 2011), reunind 25 de studii clinice mari adresate factorilor de cre[tere a coloniilor de granulocite, la pacien]i cu tumori solide sau limfoame, sa ar`tat c` pegfilgrastim (Neulasta®) reduce inciden]a FN întro m`sur` mai mare decât filgrastim (Neupogen®), [i anume riscul relativ este mai mic cu 33% (p =0,04). Rezultate similare au fost publicate [i anterior (2007), în dou` recenzii sistematice: Kuderer NM, J Clin Oncology si Pinto L, Current Med Research & Opinion.
În ciuda pa[ilor îndr`zne]i care sau f`cut în privin]a abord`rilor terapeutice, mii de pacien]i afla]i sub chimioterapie sunt înc` spitaliza]i anual din cauza episoadelor de neutropenie febril`. De aici deriv` prioritatea companiei Amgen de a trata pacien]ii eligibili, servind interesele profesionale ale corpului medical.
Pegfilgrastim (Neulasta®): 10 ani aniversari de existen]` în arsenalul terapeutic
Supliment special Conferin]a Societ`]ii Na]ionale de Oncologie Medical` din România
he worked as a special fellow at Memorial Sloan Kettering Cancer Center in New York, after which he held several positions at respectively the University Hospital Utrecht, The Netherlands Cancer Institute / Antoni van Leeuwenhoek Hospital and the VU Medical Center.
Although the concept of immune surveillance in cancer was first proposed more than 40 years ago, the recent discovery that agents that modulate immune regulatory checkpoints or target driver oncogenes can significantly improve the survival of patients with cancer, especially those with advanced malignancies, has led to a new era of innovation in oncology.
The challenge of immunotherapy is to boost the patient’s antitumor immune response by overcoming tumorinduced ‘immune editing’ and shifting the balance from protumor to antitumor immunity. The ultimate goal of immunotherapy in oncology is to utilize the immune system to eradicate and, ideally, to cure cancer.
In terms of types of cancer, the focus is on solid tumors and specifically melanoma. This reflects the pivotal role melanoma has played in the emergence and development of immunotherapies for cancer. This is a consequence, in part, of the observed spontaneous immune responses to melanoma in some patients and the ease with which melanoma cells can be cultured in vitro. It is also a function of clinical necessity, because of the recalcitrant nature of this cancer to nonimmunological therapies and older immunotherapies.
Advances in basic molecular immunology have enabled identification of new immune system targets for treating cancer, some of which have resulted in novel agents
that are in latestage clinical development. These agents, either alone or in combination, have the potential to offer real, longterm benefit to patients with advanced disease. Advances in targeted therapies (inhibitors of BRAF, MEK, cKIT, PI3K) and immunotherapy (antiPD1) are expected and will influence treatment landscape. As is mentioned in the recently issued ESMO guidelines, the role of life expectancy for patient selection at different points can be a driver of treatment decisions.
At this symposium, we will discuss new treatment approaches, review ongoing research into immunological markers for novel immunotherapies and discuss the practicalities and challenges associated with integrating novel treatments into clinical practice.

| Septembrie 201246
l Prof. Dr. Doris Henne-Bruns Head of the Department of Surgery, University of Ulm, Germany
Primary hepatocellular carcinoma (HCC) is one of the most frequently encountered solid organ tumors worldwide. The tumor is mainly observed in patients with chronic liver disease or cirrhosis, but can also develop in normal parenchyma.
For the treatment of HCC, several therapeutic options exist:
primary resection;liver transplantation;local destruction (e.g. radiofrequency ablation, etha
nol injection);transarterial chemoembolisation.The individual treatment will depend on the following
parameters:benign, malignant (safety margin);size of the tumor;number of tumors;localization within the liver;preexisting liver disease (steatosis, fibrosis, cirrhosis);estimated function of the remaining liver parenchyma
(volume of the remaining liver, length of operation, blood loss, transfusion, postoperative infections, impaired coagulation).
Colorectal liver metastases are the most common in
dication for liver resections in Europe and North America. Colorectal liver metastases occur synchronously or metachronously with the primary tumor and are resectable in about 20% of the cases. For the resection of liver metastases, the same parameters as described above have to be taken into account, prior to an operation.
The actual discussion on the treatment of colorectal liver metastases tries to answer several questions like:
which patients benefit from neoadjuvant chemotherapy, prior to liver resection?
which patients benefit from adjuvant chemotherapy after liver resection?
Surgical Strategies in Primary and Secondary Liver Tumors
REFERENCES:HCC Leitlinie Am. Ass. Study of Liver Disease , Hepatology, 42, 2005, Barcelona Clinic Liver Cancer Staging ClassificationR. Cabrera, D.R. Nelson: The Management of Hepatocellular Carcinoma. Review, Aliment Pharmakol Ther 31, 461-476, 2010N. C. Tsim et al: Surgical treatment for liver cancer. World J Gastroenterol. 16(8), 927-933, 2010,
www.revista-hipocrate.ro REZUMAT
l Doru Ghizdavescu MD
Anemia reprezint` o complica]ie frecvent` a tumorilor maligne sau a chimioterapiei [i contribuie la cre[terea mortalit`]ii [i reducerea calit`]ii vie]ii. Eritropoietina uman` recombinant` (rHuEPO) reprezint` un tratament eficace pentru anemie, la pacien]ii care primesc chimioterapie, determinând cre[terea nivelului de hemoglobin` [i reducând sau eliminând necesarul de transfuzii de mas` eritrocitar`(1, 2).
Darbepoetin alfa (Aranesp®) este singurul agent de stimulare a eritropoiezei de genera]ia a 2a înregistrat pentru tratamentul anemiei induse de chimioterapie. Aranesp® are o structur` unic` de aminoacizi, un con]inut mai mare de acid sialic în molecul`, timp de înjum`t`]ire crescut (74 de ore la pacien]ii cu cancer) [i o valoare biologic` superioar` celei a rHuEPO. Datorit` propriet`]ilor farmacocinetice diferite fa]` de rHuEPO, darbepoetina alfa se poate administra mai rar, la 3 s`pt`mâni, fa]` de administrarea s`pt`mânal` pentru epoetinele de prima genera]ie(1).
Eficacitatea administr`rii a 500 µg Aranesp® la 3
s`pt`mâni (Q3W), fa]` de administrarea s`pt`mânal` (QW) a 2,25 µg/kg corp, a fost evaluat` întrun studiu controlat randomizat(2). Administrarea Q3W a fost cel pu]in la fel de eficient` cu administrarea QW atât prin reducerea necesarului de transfuzii de mas` eritrocitar`, cât [i prin corectarea nivelului de Hb(2).
O metaanaliz` a tuturor studiilor controlate (n =6) care au evaluat eficacitatea [i siguran]a DA versus placebo a ar`tat c` Aranesp® reduce necesarul de transfuzii cu 57% versus placebo. Tratamentul cu Aranesp® nu a afectat supravie]uirea f`r` progresie (HR =0.93 (95% CI, 0,841,04)) sau supravie]uirea general` (HR =0,97 (95% CI, 0,851,10)), dar inciden]a evenimentelor tromboembolice a fost mai mare la pacien]ii trata]i cu Aranesp®(3).
Darbepoetin alfa reprezint` un tratament modern [i eficace al anemiei simptomatice indus` de chimioterapie care se poate administra la 3 s`pt`mâni.
Excelen]a în tratamentul anemiei indus` de chimioterapie
BIBLIOGRAFIEKiss Z et al. 2009; Eur J Clin PharmacolCanon JL et al. 2006; JNCILudwig H et al. 2009; JCO

Colecţia de
primăvară
2012
Publicaţie trimestrială pentru sănătatea ta
și a familiei tale
Revista 4P
Învingem cancerul!
O dată-n viaţă
Sănătatea copilului:Sănătatea copilului:
Cum luptăm cu efectele adverse
ale chimioterapiei?
O lecție de autoapărare: vaccinarea
Tulburările de creștere și dezvoltare
Sănătatea adultului:Sănătatea adultului:
Jurnalul unui supraviețuitor de infarct
Să rupem tăcerea din jurul prostatei
Osteoporoza: boala care te fură pe neștiute
Legături periculoase între inimă și creier:
fibrilația atrială și accidentul vascular cerebral
Util: Cele mai active asociaţii ale pacienţilor din România
Povesteamea
Sănătatea vârstei a treia:
Sănătatea vârstei a treia:Iuliana Tudor
Pret: 6,9 RON
Rev
ista
4p
- P
erso
nal
izar
e P
reve
nți
e Pa
rtic
ipar
e P
red
icți
e
Recomandă prietenilor tăi revista
www.pppp.ro
Apare trimestrial și poate fi găsită în magazinele Inmedio / Relay
Un produs
NOUA apărut ediția de toamnă 2012. Special Felicia Filip